Safe Acetaminophen Dose Calculator
This tool calculates your safe daily acetaminophen dose based on liver health and alcohol use. Always consult your doctor before taking any medication.
Based on your liver health and alcohol use, your safe maximum is mg per day.
Always check medication labels for hidden acetaminophen (look for "APAP" or "acetaminophen" on ingredients lists).
Acetaminophen Overdose is a Medical Emergency
Call poison control immediately at 1-800-222-1222 if:
- You've taken more than your calculated safe dose
- It's been more than 24 hours since you took acetaminophen
- You're experiencing nausea, vomiting, or abdominal pain
Don't wait for symptoms - liver damage can happen quickly.
Acetaminophen is in almost every medicine cabinet. You’ve probably taken it for a headache, fever, or sore muscles. It’s in Tylenol, in cold medicines, in prescription painkillers like Vicodin and Percocet. But if you have liver disease, or even just drink alcohol regularly, that little white pill can quietly damage your liver-sometimes with deadly results.
Why Acetaminophen Is Riskier Than You Think
Acetaminophen is safe when used exactly as directed. But the line between safe and dangerous is thin. For most people, the maximum daily dose is 4,000 milligrams. That sounds like a lot-until you realize how easy it is to hit that limit without trying.
Take two extra-strength Tylenol pills (500 mg each) every four hours. That’s 3,000 mg already. Now add a cold medicine like NyQuil or DayQuil, which also contains acetaminophen. You’ve just jumped to 4,000 mg. Do it again the next day? You’re in danger territory.
And if you have liver disease? That limit drops. Experts say 2,000 to 3,000 mg per day is safer. Some doctors recommend staying under 2,000 mg if you have cirrhosis, hepatitis, or any form of chronic liver damage. Why? Because your liver can’t process the drug the way a healthy one does.
How Acetaminophen Damages the Liver
Your liver breaks down acetaminophen in two main ways: through safe pathways that turn it into harmless waste, and a backup pathway that creates a toxic byproduct called NAPQI. Normally, your liver has enough glutathione-a natural antioxidant-to neutralize NAPQI before it causes harm.
But when you take too much acetaminophen, the safe pathways get overwhelmed. More NAPQI is made. Glutathione runs out. NAPQI starts attacking liver cells. Within hours, this can cause serious, even irreversible damage.
This isn’t just about one big overdose. It can happen slowly. Someone with chronic pain takes 3,000 mg a day for weeks. Their liver is constantly stressed. Glutathione never gets a chance to recover. Eventually, the damage adds up. That’s why repeated supratherapeutic dosing is just as dangerous as a single overdose.
Who’s Most at Risk
Not everyone who takes acetaminophen will have problems. But certain people are far more vulnerable:
- People with liver disease-Hepatitis B or C, fatty liver, cirrhosis. Their livers are already weakened and can’t handle extra stress.
- Chronic alcohol users-Even moderate drinking (3+ drinks a day) increases the risk. Alcohol makes the liver produce more of the toxic NAPQI pathway and lowers glutathione levels.
- People who are malnourished-Low protein intake or eating disorders reduce glutathione production.
- Those taking other liver-metabolized drugs-Medications like seizure drugs (phenytoin, carbamazepine) or tuberculosis drugs (isoniazid) push the liver into overdrive, making acetaminophen more toxic.
One study found that people with hepatitis C who took regular doses of acetaminophen were more likely to show signs of liver enzyme spikes-early warning signs of damage. And in patients with cirrhosis, even 2,000 mg a day can be too much.
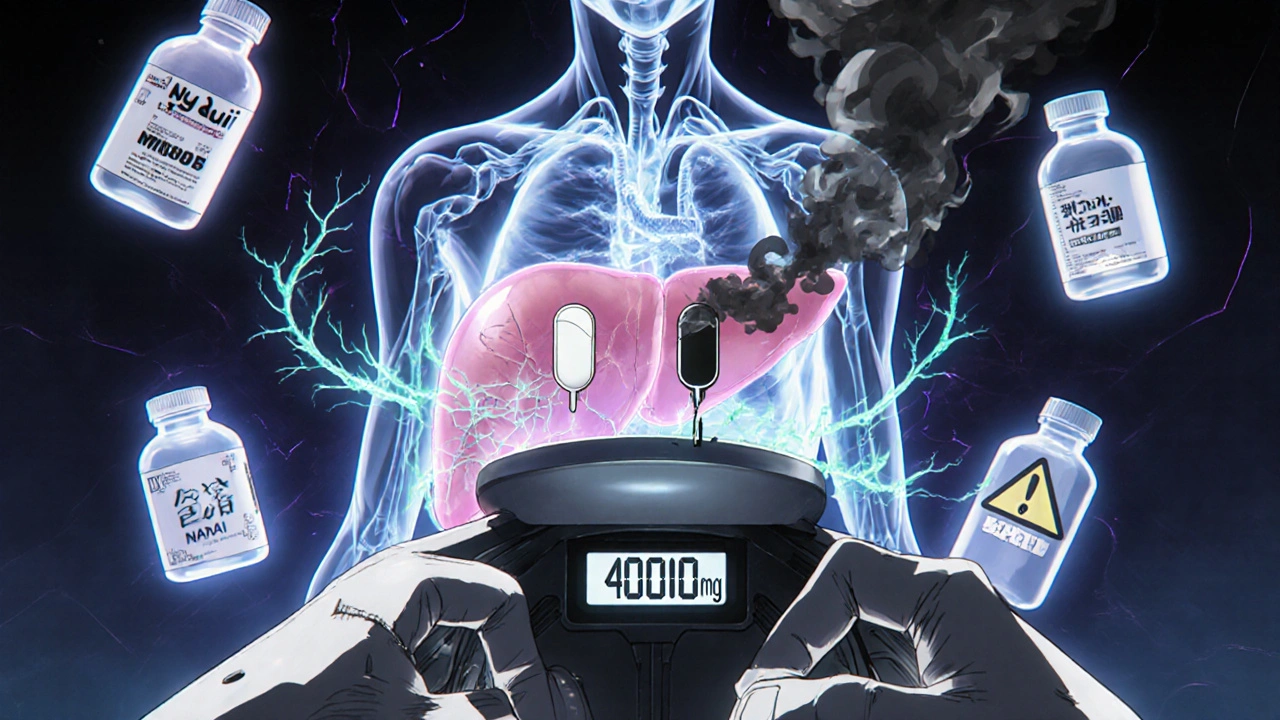
Hidden Sources of Acetaminophen
The biggest danger isn’t taking too much Tylenol. It’s taking too many things that contain acetaminophen.
Look at the label. You’ll often see it listed as “APAP” on prescription bottles. That stands for N-acetyl-para-aminophenol-the chemical name for acetaminophen. If you don’t know that, you might think you’re taking two different medicines when you’re really taking two doses of the same drug.
Common products with hidden acetaminophen:
- Vicodin, Percocet, Norco (painkillers)
- Excedrin (migraine relief)
- Midol (menstrual pain)
- Sudafed PE Cold & Flu
- NyQuil, DayQuil, Theraflu
- Many sleep aids and combination cold remedies
Always read the active ingredients. If you see “acetaminophen” or “APAP,” add it to your total. Don’t assume a “non-drowsy” or “daytime” version is safe-it might still have it.
What You Should Do If You Have Liver Disease
If you have any form of liver disease, don’t guess. Talk to your doctor. But here’s what most experts agree on:
- Stay under 2,000 mg per day-This is the safest limit for most people with liver damage.
- Avoid alcohol completely-Even one drink can push you over the edge.
- Check every medication-Every pill, syrup, or nasal spray. Write down every product you take and look up the acetaminophen content.
- Use the lowest effective dose-If 325 mg works, don’t take 650 mg.
- Don’t use it long-term-If you need pain relief for more than a few days, talk to your doctor about alternatives.
Some doctors recommend switching to non-acetaminophen pain relievers like ibuprofen or naproxen-but those carry their own risks, especially for kidneys or stomach. There’s no perfect option. The key is working with your doctor to find the safest balance.

What to Do If You Think You’ve Taken Too Much
Acetaminophen overdose is a medical emergency. But it’s treatable-if you act fast.
The antidote is acetylcysteine (NAC). It works by replenishing glutathione, helping your liver neutralize the toxic NAPQI. NAC is most effective if given within 8 hours of overdose. It still helps if given up to 16 hours later.
Don’t wait for symptoms. Nausea, vomiting, and abdominal pain often don’t show up until 24 hours after overdose-by then, liver damage may already be severe.
If you suspect you’ve taken too much:
- Call poison control immediately (1-800-222-1222 in the U.S.)
- Go to the ER-even if you feel fine
- Bring all your medications with you
Hospital staff will check your blood acetaminophen level and use the Rumack-Matthew nomogram-a chart that predicts risk based on timing and dose-to decide if you need NAC. If your dose was over 10 grams or 200 mg/kg, they’ll start NAC even before test results come back.
What About Children?
Children are more sensitive to acetaminophen. The safe dose is 10 to 15 mg per kilogram of body weight every 4 to 6 hours, with a maximum of 80 mg/kg per day.
Always use the measuring syringe that comes with the liquid medicine. A kitchen spoon can give you 2 to 3 times too much. Never use adult formulations for kids. Never mix different children’s medicines unless a doctor says it’s safe.
If a child accidentally takes too much, go to the ER right away. Don’t wait for symptoms. Children can develop liver failure faster than adults.
Bottom Line: Acetaminophen Is Not Harmless
It’s not the drug’s fault. It’s the way we use it. We treat it like candy because it’s easy to buy, doesn’t make us drowsy, and doesn’t hurt our stomach like ibuprofen. But it’s one of the most dangerous drugs in your medicine cabinet-if you have liver disease or drink alcohol.
Acetaminophen overdose causes about 500 deaths a year in the U.S. alone. Most of those are preventable. The problem isn’t bad people. It’s confusion. It’s labels that are too small. It’s assuming “natural” or “non-prescription” means “safe.”
If you have liver disease, your number one rule: When in doubt, don’t take it. Talk to your doctor. Ask for alternatives. Keep a list of everything you take. Check every label. And never mix it with alcohol.
Acetaminophen can be safe. But safety isn’t about the pill. It’s about how you use it.
Can I take acetaminophen if I have fatty liver disease?
Yes, but with strict limits. Most liver specialists recommend staying under 2,000 mg per day, even if you don’t drink alcohol. Fatty liver reduces your liver’s ability to process toxins, so the standard 4,000 mg limit is too high. Always check with your doctor before using it regularly.
Is Tylenol Extra Strength safer than regular Tylenol?
No. Tylenol Extra Strength contains 500 mg per tablet, compared to 325 mg in regular Tylenol. That means you hit the daily limit faster. The manufacturer actually recommends a maximum of 3,000 mg per day for Extra Strength, not 4,000 mg. Always follow the label on the bottle you’re using.
Does alcohol have to be binge drinking to be dangerous with acetaminophen?
No. Even moderate daily drinking-like one or two drinks a day-can increase your risk. Alcohol changes how your liver processes acetaminophen, making the toxic byproduct NAPQI form faster and reducing your body’s ability to neutralize it. There’s no safe level of alcohol when you’re taking acetaminophen regularly.
Can I take acetaminophen while pregnant if I have liver issues?
Pregnant women with liver disease should avoid acetaminophen unless a doctor says it’s necessary. While oral and IV acetylcysteine (NAC) are safe to use in pregnancy if overdose occurs, the drug itself should be minimized. Always use the lowest dose for the shortest time possible. Talk to your OB-GYN before taking any pain reliever.
What are the early signs of acetaminophen liver damage?
Early signs are often mild and easily missed: nausea, vomiting, loss of appetite, and tiredness. These can appear 12 to 24 hours after overdose. By the time jaundice (yellow skin), dark urine, or abdominal pain show up, liver damage is already advanced. If you’ve taken too much acetaminophen, don’t wait for symptoms-seek help immediately.
Are there safer pain relievers for people with liver disease?
Nonsteroidal anti-inflammatories (NSAIDs) like ibuprofen or naproxen can be options, but they carry risks for kidneys and stomach, especially in people with advanced liver disease. Acetaminophen is still often preferred because it’s less likely to cause kidney problems. The best choice depends on your specific condition. Always discuss alternatives with your doctor.



Cecily Bogsprocket
November 27, 2025 AT 08:04It’s scary how many people don’t realize they’re walking into a liver trap every time they grab a cold medicine. I had a friend who took Tylenol for her back pain and NyQuil for sleep-no idea they both had acetaminophen. She ended up in the ER with transaminitis. No drama, no yelling, just quiet, slow destruction. We need more of these warnings, not less.
It’s not about fear. It’s about awareness. And awareness doesn’t come from ads or pill bottles. It comes from people sharing stories like this.
I keep a printed list of everything I take. I even write down the milligrams. It’s a pain, but it’s saved me twice already.
Don’t wait until you’re sick to start reading labels. Start now.
And if you’re helping someone older or vulnerable? Sit with them. Go through their meds together. That’s real care.
Thank you for writing this. It’s the kind of post that changes lives.
One pill at a time, we can stop this silent epidemic.
Mira Adam
November 29, 2025 AT 06:54Stop pretending acetaminophen is safe. It’s a chemical landmine disguised as a Band-Aid. If your liver is even slightly compromised, you’re playing Russian roulette with every dose. People who say ‘I only take it occasionally’ are the ones who end up on transplant lists. Wake up. This isn’t ‘maybe dangerous’-it’s ‘guaranteed to hurt you if you’re not perfect.’ And you’re not perfect.
Stop blaming the labels. Blame the people who keep buying it like candy.
And yes, I’m talking to you, the one who takes Tylenol with a beer. You’re not a ‘moderate drinker.’ You’re a walking overdose waiting to happen.
Miriam Lohrum
December 1, 2025 AT 00:34I’ve been thinking about this a lot lately. We treat pain like a problem to be erased, not a signal to be understood. Acetaminophen doesn’t fix the cause-it just muffles the scream. And in doing so, it lets the real damage grow in silence.
What if we stopped reaching for pills the moment we felt discomfort? What if we learned to sit with pain, to move differently, to rest more, to breathe deeper? Maybe then we wouldn’t need to poison our livers just to feel okay.
It’s not anti-medical. It’s anti-quick-fix.
There’s something deeply human about this. We want relief without responsibility. But the body doesn’t work that way.
Just food for thought.
Edward Batchelder
December 1, 2025 AT 20:43Thank you for this. Seriously. This is the kind of information that should be taught in high school health class, not buried in a PDF only doctors read.
I’ve worked with elderly patients for over 20 years, and I’ve seen too many of them take 10 pills a day without knowing what’s in them. One man took Vicodin, DayQuil, and Excedrin every night. He thought he was ‘just managing pain.’ He didn’t know he was slowly killing his liver.
Education is the antidote. Not just to acetaminophen, but to the culture of ‘take it and forget it.’
Let’s push for clearer labeling. Let’s demand pharmacy counseling. Let’s make this part of every prescription. Because no one should die because they didn’t know what APAP meant.
And if you’re reading this and you’ve never checked a label? Do it today. Your liver will thank you.
One small step at a time.
-E.B., RN
reshmi mahi
December 3, 2025 AT 05:53LOL Americans think they're smart because they read labels? In India we just take whatever the pharmacy gives us and call it a day. And guess what? We don't die from acetaminophen. We die from pollution, poor sanitation, and corrupt doctors. This is a first-world problem wrapped in a guilt-trip.
Also, who even reads labels? I just look for the blue pill. 🤷♀️💊
laura lauraa
December 3, 2025 AT 14:10While I appreciate the intention behind this post, I must respectfully yet firmly object to the implicit moralization of pharmaceutical use. The assertion that ‘acetaminophen is dangerous’ is an oversimplification that ignores the nuanced pharmacokinetics of hepatic metabolism, particularly in the context of genetic polymorphisms in CYP2E1 activity, which vary significantly across ethnic populations. Furthermore, the conflation of ‘alcohol use’ with ‘liver disease’ is clinically misleading; moderate consumption does not equate to steatosis, nor does it necessarily impair glutathione synthesis in the absence of pre-existing pathology. The recommendation to ‘avoid alcohol completely’ is not evidence-based for all populations, and may, in fact, contribute to unnecessary anxiety and therapeutic nihilism among patients with compensated cirrhosis. The author’s tone, while well-intentioned, borders on alarmist and lacks the precision required for responsible medical communication. I would urge greater nuance, peer-reviewed citations, and a reduction in emotionally charged language such as ‘quietly damage’ and ‘deadly results,’ which, while evocative, are not diagnostic terms. This is not fear-mongering-it is fear-misinformation.
Gayle Jenkins
December 5, 2025 AT 13:18Hey, I’m a nurse and I’ve seen this too many times. People think ‘natural’ means safe. It doesn’t. Acetaminophen is a toxin. Period. But here’s the good news: you can protect yourself. You don’t need to suffer. You don’t need to guess.
Here’s what you do: write down every pill you take. Every. Single. One.
Then go to Drugs.com or MedlinePlus. Type in each one. Look for APAP or acetaminophen. Add them up.
If you’re over 2,000 mg, stop. Talk to your doctor. Ask for ibuprofen, ask for physical therapy, ask for a referral to pain management.
And if you’re drinking? Stop. Even one drink a day is a gamble you don’t need to take.
You’re not weak for needing pain relief. You’re smart for asking how to do it safely.
I’ve helped dozens of people avoid liver failure. You can too. Just start today. One label at a time.
Kaleigh Scroger
December 6, 2025 AT 07:07Let me give you the real deal from someone who’s worked in hepatology for 15 years. The 2,000 mg limit isn’t arbitrary-it’s based on multiple studies showing that patients with NAFLD or early cirrhosis develop transaminitis at doses as low as 1,500 mg daily when combined with even occasional alcohol. The glutathione depletion isn’t linear-it’s exponential once you cross the threshold. And here’s the kicker: most patients don’t even know they have fatty liver until it’s stage 3. That’s why we tell everyone to assume they have it until proven otherwise.
Also, NAC isn’t just for overdoses. There’s emerging data that low-dose daily NAC (600 mg) may help protect the liver in high-risk patients on chronic acetaminophen, though it’s not yet standard of care. Talk to your doctor about it.
And yes, NSAIDs aren’t perfect. They cause GI bleeds and renal impairment. But in advanced cirrhosis, they’re often worse. So it’s a tradeoff. The goal isn’t to avoid all meds-it’s to avoid the ones you don’t need. If you’re taking acetaminophen for tension headaches three times a week? Try yoga. Or a hot shower. Or just lying down for 10 minutes. Your liver will thank you more than any pill ever could.
And if you’re on multiple meds? Get a med sync. Talk to your pharmacist. They’re the unsung heroes of this whole mess.
Bottom line: don’t be a hero. Be careful. Your liver doesn’t have a voice. You have to speak for it.