Do Doctors Even Know How Much Medications Cost?
Imagine prescribing a pill that costs $4 at one pharmacy and $320 at another - and not knowing which is which. For many clinicians, this isn’t hypothetical. It’s daily reality. Despite prescribing thousands of drugs each year, most doctors have no reliable sense of what those medications actually cost patients. Studies show they overestimate cheap drugs by 31% and underestimate expensive ones by 74%. That’s not just a minor oversight. It’s a systemic blind spot with real consequences: patients skipping doses, skipping refills, or going into debt because their doctor didn’t know a cheaper alternative existed.
The problem isn’t that doctors don’t care. In fact, 92% of surveyed physicians say they want cost information at the point of care. But they can’t get it. Not easily. Not reliably. Not in real time. The system doesn’t give them the tools. And without those tools, cost-conscious prescribing becomes an ideal - not an everyday practice.
What We Know About Clinicians’ Drug Price Knowledge
A 2016 study of 254 medical students and doctors found only 5.4% of generic drug prices and 13.7% of brand-name drug prices were estimated within 25% of the actual cost. That means more than 8 out of 10 times, a doctor’s guess about a drug’s price was way off. Generic drugs - often the cheapest option - were overestimated 77.5% of the time. Meanwhile, expensive brand-name drugs were underestimated nearly half the time. This isn’t about ignorance. It’s about information gaps.
Even experienced doctors aren’t much better. One study found that while doctors were slightly better than medical students at identifying sources of drug pricing data (84% vs. 40%), their actual estimates were still wildly inaccurate. Medical students improved slightly as they progressed through school, but their median score on a 10-question drug pricing quiz was just 6 out of 10. And here’s the kicker: fewer than half of students understood that drug prices have almost nothing to do with research and development costs. Most people - including doctors - still believe high prices mean high innovation. That’s not true. And it’s costing patients.
Why This Gap Exists
Drug pricing in the U.S. is a maze. The same medication can cost $15 at Walmart, $89 at a local pharmacy, and $320 at a hospital outpatient clinic - all depending on the patient’s insurance, pharmacy network, and whether they’ve met their deductible. There’s no single price. No public database. No simple lookup. Even Medicare Part D formularies, which many doctors rely on, are outdated, confusing, and often don’t reflect out-of-pocket costs.
On top of that, most medical schools don’t teach drug pricing. A 2021 study found 56% of U.S. medical schools have no formal curriculum on prescription costs. Students graduate knowing how a drug works - but not how much it costs. They learn pharmacology, not pricing logic. And when they enter practice, they’re expected to make cost-aware decisions without ever having been trained to do so.
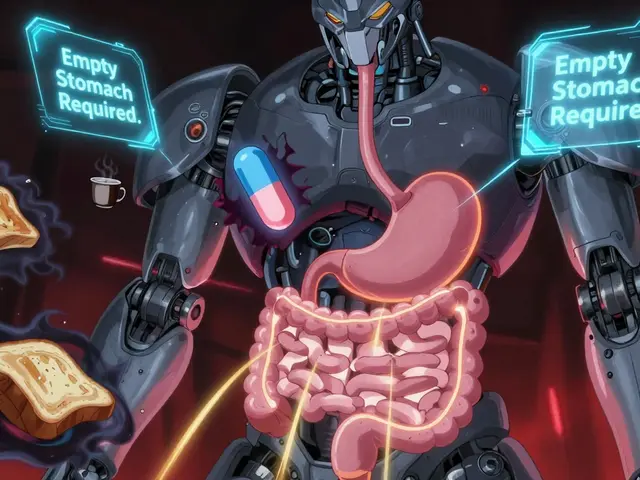
Plus, time is tight. One primary care physician on Reddit said checking drug costs takes 3 to 5 minutes per prescription. In a 15-minute appointment slot, that’s not just inconvenient - it’s impossible. Without integrated tools, doctors either guess, default to familiar brands, or skip the question entirely.

How EHRs Are Starting to Fix This
The biggest breakthrough in recent years has been electronic health record (EHR) cost alerts. Systems like Epic and Cerner now have the ability to show real-time out-of-pocket costs at the moment a doctor clicks “prescribe.” It’s not perfect - some alerts show insurer-specific prices but ignore patient-specific copays - but they’re making a difference.
A 2021 JAMA Network Open study found doctors with access to cost data in their EHRs performed significantly better on cost estimation tasks. Even more telling: one in eight primary care physicians changed a prescription after seeing a cost alert. That number jumped to one in six when the potential savings were over $20. At UCHealth, after implementing a real-time benefit tool, 12.5% of prescriptions were modified based on cost alerts. That’s thousands of patients getting cheaper, equally effective meds.
But adoption is still low. Only 37% of U.S. health systems have these tools in place as of late 2024. And they’re expensive to build - UCHealth spent $2.3 million and 18 months developing theirs. Smaller clinics can’t afford that. So the gap persists, especially in safety-net hospitals serving low-income patients.
Who’s Most Affected - And Who’s Most Likely to Change
Patients on fixed incomes, chronic conditions, or multiple medications are hit hardest. One in four adults reports skipping doses because of cost. But it’s not just about affordability - it’s about trust. If a doctor prescribes a $500 drug without mentioning a $15 alternative, patients assume the expensive one is better. That’s the invisible bias in play.
Doctors under 40 are more likely to adopt cost-aware tools. One study found 78% of younger physicians regularly use cost alerts, compared to just 52% of those over 55. That generational shift matters. Younger clinicians grew up with digital tools. They expect data at their fingertips. They’re also more likely to have been exposed to value-based care training.
Meanwhile, high-performing institutions like Mayo Clinic have created internal Drug Cost Resource Guides - updated quarterly, rated 4.7 out of 5 by users. These aren’t just lists. They’re decision aids: “This generic works just as well. Costs $12. Brand is $140.” Simple. Clear. Actionable. But they’re rare.
What’s Changing - And What’s Not
The Inflation Reduction Act of 2022 changed the game. For the first time, Medicare can negotiate prices for a handful of high-cost drugs. Public support is overwhelming - 83% of Democrats and 76% of Republicans back it. That’s not just politics. It’s pressure. Manufacturers can’t keep raising prices without consequences. Humira’s price jumped 4.7% in 2023 - with no new clinical benefit. That kind of move is now under scrutiny.
CMS now requires drugmakers to report estimated out-of-pocket costs. That data will eventually feed into EHRs. It’s slow. But it’s coming.
And the research is shifting. Earlier studies focused on whether doctors knew absolute prices. Now, the focus is on value: Is this drug worth the cost? Is there a cheaper alternative with the same effect? The Institute for Clinical and Economic Review is leading this shift, pushing systems to evaluate not just price, but clinical benefit.
Still, the biggest barrier remains: education. No amount of tech will fix this if doctors aren’t trained to use it. And right now, most aren’t.
What Needs to Happen Next
Three things are critical:
- Make cost data mandatory in EHRs. Every prescription screen should show estimated out-of-pocket cost before the doctor clicks “send.” No opt-in. No toggle. Just the information.
- Teach drug pricing in med school. It’s not a niche topic. It’s part of prescribing. Every student should learn how to compare alternatives, understand formularies, and explain cost trade-offs to patients.
- Standardize pricing transparency. The same drug shouldn’t cost $15 at one pharmacy and $320 at another. There needs to be a baseline - even if insurance changes the final number - so doctors and patients can make informed choices.
The data is clear: when doctors know the cost, they prescribe better. Patients take their meds. Health improves. Costs drop. One 2023 study found cost-transparency tools reduced patient out-of-pocket spending by $187 per person annually. That’s not a rounding error. That’s life-changing.
Doctors want to help. Patients want affordable care. The tools exist. The evidence is solid. The question isn’t whether we can fix this. It’s whether we’re willing to.
Do most doctors know how much medications cost?
No. Studies show most clinicians overestimate the cost of cheap drugs and underestimate expensive ones. Only about 5% of generic drug prices and 14% of brand-name drug prices are estimated within 25% of the actual cost. This isn’t due to lack of concern - it’s because reliable, real-time pricing data isn’t available at the point of care.
Why don’t doctors know drug prices?
Drug pricing in the U.S. is fragmented and opaque. The same medication can cost $15 at one pharmacy and $320 at another, depending on insurance, pharmacy networks, and deductibles. There’s no central database. Most medical schools don’t teach drug pricing. And EHRs often don’t show real-time patient-specific costs. Doctors are left guessing - or ignoring the issue entirely.
Can EHR cost alerts help doctors prescribe more affordably?
Yes. When EHRs show real-time out-of-pocket costs, one in eight doctors change their prescription - and that number rises to one in six when savings exceed $20. Systems like UCHealth’s have seen 12.5% of prescriptions modified after cost alerts. But only 37% of U.S. health systems have these tools installed.
Is there a difference in cost awareness between medical students and doctors?
Doctors are slightly better at identifying sources of pricing data (84% vs. 40% of students), but both groups are poor at estimating actual prices. Students improve slightly with experience, but their average score on a 10-question quiz is only 6 out of 10. Neither group is well-trained in pricing - and that gap doesn’t close on its own.
Are generic drugs really cheaper than brand-name drugs?
Yes - and dramatically so. In most cases, generics are 80-85% cheaper than brand-name versions and have the same active ingredients. But doctors often overestimate their cost by nearly 80% and assume brand-name drugs are more effective. This misconception leads to unnecessary spending and poorer adherence among patients.
What’s being done to improve cost awareness among clinicians?
The Inflation Reduction Act allows Medicare to negotiate prices for some drugs. CMS now requires drugmakers to report out-of-pocket cost estimates. Some institutions like Mayo Clinic offer internal cost guides. And research is pushing EHRs to integrate real-time benefit tools. But widespread adoption is still slow, and medical education on pricing remains inconsistent.


Nick Naylor
November 20, 2025 AT 14:24Let’s be brutally honest: the system is broken because we’ve outsourced medical decision-making to corporate actuaries who don’t give a damn about clinical outcomes. Doctors aren’t pharmacists-they’re not trained to navigate a price labyrinth designed to extract maximum profit. And yet, we demand they become cost-conscious arbiters without providing the tools. This isn’t negligence; it’s institutional sabotage. EHRs must embed real-time cost data-no opt-out, no toggle, no excuses. If we’re serious about value-based care, then cost transparency isn’t optional-it’s foundational. The fact that only 37% of systems have this? That’s not a technical gap. That’s a moral failure.
Brianna Groleau
November 22, 2025 AT 01:35I just want to say how deeply heartbreaking it is that we’ve created a system where a doctor has to guess whether their patient can afford the medicine they’re prescribing-like it’s some kind of cruel lottery. I’ve seen my grandmother skip her insulin because the pharmacy said $400, and her doctor never knew there was a $12 generic. It’s not just about data-it’s about dignity. When we treat health like a market commodity instead of a human right, we break trust. And trust? Once it’s gone, no algorithm can rebuild it. We need to teach this in med school, yes-but more than that, we need to rebuild the soul of medicine. It’s not about saving money. It’s about saving lives. And it starts when we stop pretending that price doesn’t matter.
Bill Camp
November 23, 2025 AT 21:24Everyone’s acting like this is a new problem. Newsflash-it’s not. The drug industry has been gaming this system for decades. You think doctors are the problem? Look at the pharma reps who hand out free samples of $500 drugs while the $15 generic sits on the shelf. You think EHR alerts are the solution? They’re a Band-Aid on a hemorrhage. The real fix? Break the monopoly. Let generics compete. Let Medicare negotiate. Let patients see the real price before they even walk into the pharmacy. Until then, we’re just rearranging deck chairs on the Titanic.
Lemmy Coco
November 24, 2025 AT 16:19i just read this and thought… wow. i mean, i know doctors are busy but like… how do they not know? i had a friend who got prescribed something and the pharmacy said $300 and she cried because she was on disability and the doc had no idea there was a $12 version. i think ehrs should just auto-pop the cost. like, why is this even a debate? it’s 2025. we have apps that tell us the price of avocados. why can’t our medical software tell us the price of pills? also i think med schools should have a class called ‘how not to bankrupt your patients’ lol
rob lafata
November 26, 2025 AT 10:49Oh wow, another bleeding-heart liberal fantasy about ‘cost transparency.’ Let me guess-you also think doctors should be forced to prescribe only generics because ‘it’s cheaper.’ Newsflash: not every generic is equal. Some are manufactured in questionable facilities. Some have bioavailability issues. And you think a 15-second EHR pop-up is going to replace 10 years of clinical judgment? You’re not just naive-you’re dangerous. The real issue? Patients want the best, not the cheapest. And if you’re too lazy to pay for quality, that’s your problem-not the doctor’s. Stop punishing clinicians for a broken system they didn’t create.
Matthew McCraney
November 27, 2025 AT 16:47They’re lying. This whole thing is a psyop. The ‘cost alerts’? They’re not real. They’re planted by Big Pharma to make you think they’re trying to help while they jack up prices behind the scenes. The FDA, CMS, Epic-they’re all in on it. You think doctors don’t know prices? They know EXACTLY what’s going on. They’re paid off. The ‘$15 generic’? It’s probably laced with talc or worse. The real solution? Burn the system down. No more EHRs. No more pharmacies. No more drugs. Just herbs, sunshine, and fasting. That’s what they don’t want you to know. They’re scared of people waking up.
serge jane
November 28, 2025 AT 16:48What we're really talking about here is the erosion of care into transaction. The moment medicine became a commodity, we lost something essential. Doctors used to know their patients-not just their labs, but their lives. Now they’re clicking buttons in a system designed to maximize efficiency, not humanity. Cost awareness isn’t just about numbers-it’s about presence. Can you imagine prescribing a drug without knowing if your patient will eat this month? That’s the context we’ve erased. The tools help-but they’re not the cure. The cure is returning to the relationship. The doctor. The patient. The trust. Everything else is just noise.
swatantra kumar
November 29, 2025 AT 10:28Bro, this is wild 😅 In India, we get generics for $0.50 and doctors just say ‘take this, it’s the same.’ No EHR needed. Just common sense. But here? You need a PhD in insurance to get a $12 pill. The system is literally designed to confuse. And yet… people still trust doctors. That’s the real miracle. 🙏
Cinkoon Marketing
November 29, 2025 AT 20:52Actually, you’re all missing the bigger picture. The real issue is that medical education hasn’t kept up with healthcare economics. But here’s the thing-doctors aren’t the only ones who need training. Patients need to understand that price ≠ quality. And pharmacies? They’re the worst offenders. Why does CVS charge $200 for a drug that Walmart sells for $15? That’s price gouging, plain and simple. And until we regulate pharmacy benefit managers like we regulate utilities, nothing’s going to change. Also, why is this even a debate? It’s 2025. We have price comparison apps for everything else. Why not meds?