Antabuse vs Alternatives: Medication Selector
Your Drinking Pattern
Health Status
Motivation Level
Other Considerations
Recommended Medication
Key Takeaways
- Antabuse works by creating unpleasant reactions to alcohol, while most alternatives block cravings or reduce reward.
- Effectiveness varies: Antabuse is best for highly motivated patients, Naltrexone shines for reducing heavy‑drinking lapses, and Acamprosate helps maintain abstinence.
- Safety profiles differ - Antabuse can cause liver toxicity, Naltrexone may affect the liver moderately, and Acamprosate is gentle on the liver.
- Choosing the right medication hinges on personal health, drinking patterns, and whether you can stick to a strict dosing schedule.
- Regular monitoring and combining medication with counseling dramatically improves success rates.
Why a Comparison Matters
When you or a loved one decides to quit drinking, the first question is usually, “Which medication will work best for me?” Antabuse comparison searches spike every year because people want a side‑by‑side look at the options. Understanding how each drug works, its pros and cons, and who it’s best suited for can turn a vague hope into a concrete plan.
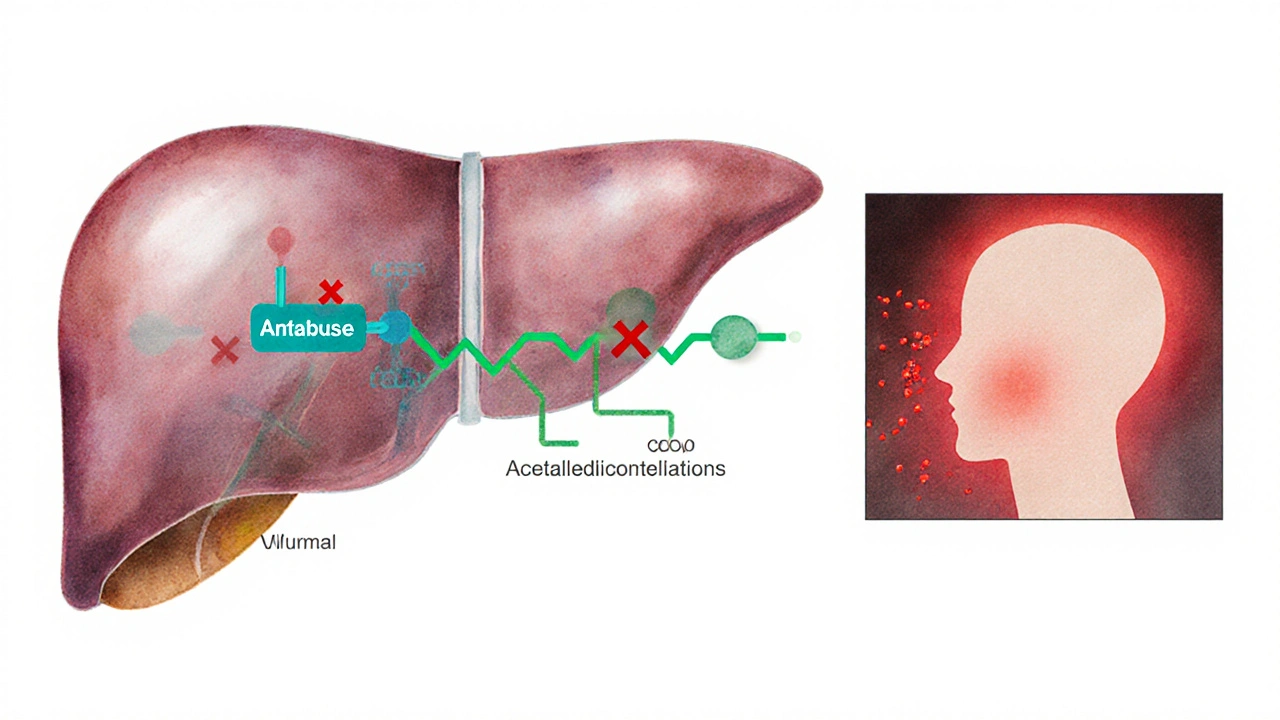
Antabuse (Disulfiram) - How It Works
Antabuse is a once‑daily oral medication that inhibits aldehyde dehydrogenase, the enzyme that breaks down acetaldehyde after alcohol consumption. When a person drinks while taking Antabuse, acetaldehyde builds up, causing flushing, nausea, vomiting, headache, and rapid heartbeat. The reaction starts within 10 minutes and can last for an hour or more, creating a strong deterrent.
Key attributes of Antabuse:
- Typical dose: 250mg once daily.
- Onset of deterrent effect: Immediate after dosing.
- Required monitoring: Liver function tests at baseline and every 2-3 months.
- Best for: Highly motivated patients who can adhere to a strict regimen and avoid alcohol completely.
Major Alternatives at a Glance
Besides Antabuse, clinicians often prescribe other FDA‑approved medications for Alcohol Use Disorder (AUD). Below are the most common choices.
Naltrexone is a opioid receptor antagonist that reduces the rewarding feelings of alcohol. It comes in oral (50mg daily) and injectable (380mg monthly) forms.
Acamprosate is a modulator of glutamate neurotransmission that helps restore brain chemical balance after cessation. Standard dose is 666mg three times daily.
Topiramate is an anticonvulsant that also lowers alcohol cravings by affecting GABA and glutamate pathways. Dosing starts at 25mg and may increase to 200mg daily.
Gabapentin is a gamma‑aminobutyric acid analogue that eases withdrawal symptoms and reduces cravings in some patients. Typical regimen: 300mg three times daily, titrated up.
Baclofen is a GABA‑B receptor agonist that dampens the urge to drink, especially in patients with liver disease. Starting dose: 5mg three times a day, can rise to 30mg three times a day.
All these drugs fall under the broader umbrella of Medication Assisted Treatment (MAT) for AUD, which pairs pharmacotherapy with counseling and behavioral support.
Side‑Effect Profiles at a Glance
Understanding safety is as crucial as efficacy. Below is a quick snapshot of common adverse events.
| Medication | Mechanism | Typical Dose | Common Side Effects | Best For |
|---|---|---|---|---|
| Antabuse | Inhibits aldehyde dehydrogenase | 250mg daily | Flushing, nausea, liver enzyme elevation | Highly motivated, can avoid alcohol |
| Naltrexone | Opioid receptor antagonist | 50mg daily or 380mg IM monthly | Headache, dizziness, mild liver impact | Those who need craving control |
| Acamprosate | Glutamate modulator | 666mg three times daily | Diarrhea, abdominal pain | Maintaining abstinence after detox |
| Topiramate | GABA‑enhancer, glutamate inhibitor | Start 25mg, up to 200mg daily | Paresthesia, cognitive slowing, kidney stones | Heavy drinkers with strong cravings |
| Gabapentin | Calcium channel modulator | 300mg TID, titrate to 600mg TID | Drowsiness, edema, weight gain | Patients with withdrawal anxiety |
| Baclofen | GABA‑B agonist | 5mg TID, up to 30mg TID | Muscle weakness, sedation, hypotension | People with liver disease or contraindication to other meds |
Decision Factors You Should Weigh
Choosing a medication isn’t a one‑size‑fits‑all exercise. Below are the top criteria patients and clinicians typically evaluate.
- Efficacy for the specific drinking pattern. Antabuse works best for total abstinence enforcement. Naltrexone reduces heavy‑drinking days, while Acamprosate helps sustain abstinence after detox.
- Safety and liver health. If you have existing liver disease (common in long‑term alcohol users), Antabuse and Naltrexone require close monitoring. Acamprosate is renally cleared and spares the liver, making it a safer pick for hepatic impairment.
- Adherence potential. Antabuse's once‑daily dosing seems simple, but the need to avoid all alcohol can feel restrictive. Oral Naltrexone also needs daily intake, whereas the injectable version eliminates adherence gaps.
- Interaction with other meds. Topiramate and Gabapentin can lower seizure thresholds when combined with certain drugs. Baclofen may intensify the effects of other CNS depressants.
- Cost and insurance coverage. In many health systems, generic Antabuse and Naltrexone are inexpensive, while extended‑release Naltrexone injections and Topiramate can be pricier.

Putting It All Together: Which Option Fits You?
Here’s a quick guide based on typical patient profiles.
- Motivated, can stay completely alcohol‑free: Antabuse.
- Heavy weekend binge drinker seeking reduced cravings: Oral or injectable Naltrexone.
- Someone who completed detox and wants to stay sober: Acamprosate.
- Patient with strong cravings and partial response to first‑line meds: Topiramate (off‑label) or Gabapentin.
- Liver disease or contraindication to other drugs: Baclofen.
Regardless of the choice, pairing medication with evidence‑based counseling (Cognitive Behavioral Therapy, Motivational Enhancement, or 12‑step facilitation) boosts quit rates from ~30% to 60%+.
Monitoring and Managing Risks
All MATs for AUD demand regular follow‑up:
- Baseline liver function tests (ALT, AST) for Antabuse and Naltrexone.
- Renal function check for Acamprosate (creatinine clearance).
- Blood pressure and electrolyte monitoring for Baclofen.
- Assess side‑effects at each visit; adjust dose or switch meds if intolerable.
Patients should also receive education on potential drug‑alcohol interactions. Even a tiny sip can trigger severe Antabuse reactions, while Naltrexone can blunt the euphoric effect, reducing the desire to drink.
Frequently Asked Questions
Can Antabuse be used with other AUD medications?
Mixing Antabuse with another medication isn’t typically recommended because the disulfiram reaction can mask side‑effects of the other drug. In practice, clinicians often pick one primary medication and add psychosocial support instead of stacking drugs.
How long does it take for Antabuse to start working?
Antabuse begins to inhibit aldehyde dehydrogenase within a few hours of the first dose, but the deterrent effect only appears when alcohol is consumed. Patients usually notice the reaction after the first drinking episode while on the medication.
Is Acamprosate safe for people with kidney problems?
Acamprosate is cleared by the kidneys, so reduced renal function can lead to drug accumulation. Dose adjustment or an alternative medication is advised for patients with a creatinine clearance < 30mL/min.
Can I stop taking Antabuse abruptly?
Because Antabuse’s effect persists for several days after a dose, stopping suddenly doesn’t cause withdrawal. However, patients should discuss any discontinuation with their prescriber to plan a safe transition to another therapy if needed.
Which medication works fastest for reducing cravings?
Injectable Naltrexone often shows a rapid drop in cravings within the first week of treatment. Oral Naltrexone and Acamprosate may take 2‑4 weeks to reach full effect.
Next Steps for Readers
If you’re considering medication‑assisted recovery, start by:
- Talking to a healthcare professional about your drinking pattern, liver/kidney health, and any other meds you take.
- Getting baseline labs (LFTs, renal panel) to narrow safe options.
- Choosing a medication that matches your motivation level and health status.
- Signing up for regular follow‑up appointments and a counseling program.
Remember, no pill works in isolation. The combination of medication, therapy, and a supportive environment offers the highest chance of long‑term sobriety.

Sruthi V Nair
October 8, 2025 AT 17:31If you want a clear path match your drinking pattern with a drug that fits your motivation level
Mustapha Mustapha
October 13, 2025 AT 16:15I see the table you posted and it lines up well with what most clinicians recommend for patients who can stick to a schedule
Ben Muncie
October 18, 2025 AT 14:59Antabuse is only useful if you truly hate the taste of alcohol after a few minutes of nausea
kevin tarp
October 23, 2025 AT 13:44The reaction latency you mentioned is accurate; the aldehyde buildup starts within ten minutes of drinking
ravi kumar
October 28, 2025 AT 11:28When you consider national health priorities the drug that harms the liver the least should be front‑and‑center. Disulfiram’s hepatic load makes it a poor first‑line choice for many.
SandraAnn Clark
November 2, 2025 AT 10:12The safety data is pretty simple. Choose the one with fewer side effects.
Rex Wang
November 7, 2025 AT 08:56In practice, the monitoring schedule you mentioned-baseline LFTs and repeat every three months-helps catch any elevation early, and patients appreciate the clear timeline, which boosts compliance
mark Lapardin
November 12, 2025 AT 07:40The pharmacokinetic profiles differ markedly: Disulfiram is metabolized hepatically, Naltrexone has both oral and depot options, while Acamprosate is renally cleared; matching the route to the patient’s organ function optimizes outcomes.
Barry Singleton
November 17, 2025 AT 06:25When evaluating Antabuse against the other FDA‑approved options, the first factor to consider is the underlying pharmacodynamics.
Disulfiram irreversibly inhibits aldehyde dehydrogenase, leading to a buildup of acetaldehyde that produces an acute aversive response.
Naltrexone, by contrast, blocks μ‑opioid receptors and dampens the rewarding sensation associated with ethanol consumption.
Acamprosate works downstream by modulating glutamatergic transmission, thereby stabilizing neuronal excitability during early abstinence.
Topiramate and gabapentin both act on GABAergic pathways, but they carry risks of cognitive slowing and sedation respectively.
Baclofen’s GABA‑B agonism is particularly advantageous for patients with compromised hepatic function because it bypasses hepatic metabolism.
From a safety perspective, liver enzyme monitoring is mandatory for both Disulfiram and Naltrexone, while Acamprosate is primarily renally cleared.
Renal impairment thus contraindicates high‑dose Acamprosate but does not affect the pharmacokinetics of Disulfiram.
Adherence is another decisive variable; a daily pill may be missed, whereas the monthly injectable formulation of Naltrexone eliminates daily decision points.
However, the injectable version incurs higher out‑of‑pocket costs and may be limited by insurance formularies.
In terms of efficacy, meta‑analyses show that Antabuse yields the highest abstinence rates among highly motivated individuals who can tolerate the severe deterrent effect.
Conversely, Naltrexone demonstrates modest reductions in heavy‑drinking days across a broader patient population.
Acamprosate shines in maintaining abstinence after detox but does not significantly curb cravings during active drinking phases.
For patients with concurrent liver disease, Baclofen remains the safest option, though its sedative profile warrants careful dose titration.
Ultimately, the optimal medication is chosen by aligning the drug’s mechanism, side‑effect profile, and dosing convenience with the patient’s drinking goals and comorbid conditions.
Javier Garcia
November 22, 2025 AT 05:09The dosing flexibility of baclofen makes it a practical alternative for patients who can’t take daily pills
christian quituisaca
November 27, 2025 AT 03:53Great point! Pairing the medication with cognitive‑behavioral therapy creates a synergistic effect, turning a modest reduction in cravings into a lasting recovery story.
Donnella Creppel
December 2, 2025 AT 02:37Wow-what a dazzling showcase of pharmacology!; the way you lay out the side‑effects reads like a blockbuster script, yet the occasional typo adds a charming human touch-truly unforgettable!
Jarod Wooden
December 7, 2025 AT 01:21Look, the data says it plainly: if you can’t tolerate liver stress, pick baclofen or gabapentin now.
lee charlie
December 12, 2025 AT 00:06Stay hopeful, the right medication can tip the scales toward sobriety, just keep the follow‑ups regular
Greg DiMedio
December 16, 2025 AT 22:50Oh sure, because taking a pill every day is exactly what everyone loves doing.
Badal Patel
December 21, 2025 AT 21:34Esteemed colleagues, permit me to elucidate the salient distinctions among the therapeutic agents; whilst Disulfiram imposes a formidable aversive response-indeed, a veritable crucible of compliance-it concomitantly exacts hepatic vigilance; Naltrexone, with its bifurcated oral and depot formulations, offers a nuanced avenue, albeit at heightened fiscal implication; Acamprosate, albeit renal‑dependent, affords a gentle maintenance strategy; regrettably, the literature intimates that topiramate’s cognitive sequelae warrant circumspection; thus, the practitioner must, with judicious exactitude, align pharmacologic choice to hepatic, renal, and psychosocial parameters, lest we falter in our fiduciary duty to the patient.
KIRAN nadarla
December 26, 2025 AT 20:18The analytic lens reveals that while Baclofen’s safety profile shines for hepatic impairment, its sedative propensity cannot be ignored; clinicians should therefore titrate cautiously, monitor blood pressure, and educate patients about potential dizziness, ensuring a balanced risk‑benefit calculus.
Kara Guilbert
December 31, 2025 AT 19:02Im really think that Acamprosate is iimportant because it dont harm the liver but dont forget the kidney check
Sonia Michelle
January 5, 2026 AT 17:47Thanks for sharing this, Sonia! Your friendly tone makes the info easy to digest and encourages anyone reading to explore treatment options with confidence.
Neil Collette
January 10, 2026 AT 16:31Oh wow, another "expert" telling us to pick the shiny new drug-because we all love spending extra cash for the same modest benefit.