When you pick up a new prescription, you might not think about what happens after it’s approved. But drugs don’t stop being monitored once they hit the shelf. The FDA safety communications are how the U.S. Food and Drug Administration tells you and your doctor about new risks that show up after a medication is already in use. These aren’t just paperwork-they’re life-saving updates. And if you don’t know how to read them, you could miss something critical.
What Are FDA Safety Communications?
FDA safety communications are official notices about new safety information on medications that are already on the market. They’re not warnings about bad batches or manufacturing errors. They’re about risks that only become clear after thousands or millions of people have used the drug. Maybe it causes rare heart problems. Maybe it interacts dangerously with another common medicine. Maybe it’s more addictive than originally thought.
The FDA started issuing these more regularly after 2007, when Congress gave them stronger powers to track drug safety after approval. Since then, they’ve issued 50 to 70 major safety communications every year. These aren’t random emails or blog posts. They’re formal, structured documents with specific sections you need to know how to read.
The Four Key Sections You Must Check
Every FDA safety communication follows the same format. If you skip parts, you’ll miss the most important details. Here’s what to look for:
- What Safety Concern Is FDA Announcing? This is the headline. It tells you in plain language what the new risk is. For example, “FDA warns that certain opioid medications can cause serious harm if stopped too quickly.” Don’t skip this. It’s written for patients and providers alike.
- For Health Care Professionals This section has the technical details: which prescribing sections changed, what the new language is, and whether it affects all drugs in a class or just one brand. It includes references like “Section 2.x, 5.x” - these point to exact spots in the official prescribing information. If you’re a doctor or pharmacist, this is where you act.
- For Patients This is your section. It tells you what to do. It might say: “Don’t stop taking this medicine on your own.” Or: “Talk to your doctor before your next refill.” It’s written in simple language, but you still need to read it carefully.
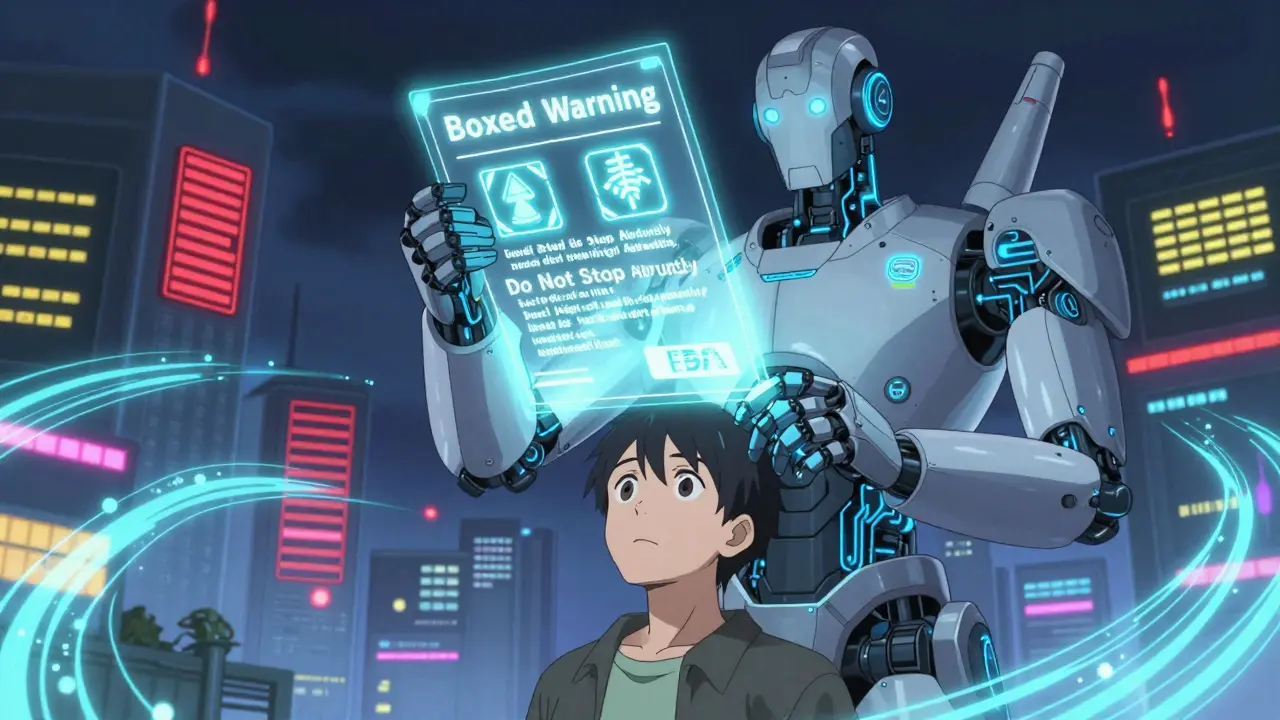
- Highlights of Prescribing Information This is a summary of the most serious changes. Look for anything marked as a “Boxed Warning.” That’s the FDA’s highest alert level. It means the risk is severe enough to be printed in a bold, bordered box at the top of the drug’s official prescribing guide.
How to Spot the Real Danger vs. Just a Reminder
Not every safety update means you need to stop your medicine. The FDA uses clear language to tell you how urgent it is.
If you see phrases like:
- “STOP using this medication immediately”
- “Do not prescribe to patients with [condition]”
- “Boxed Warning updated”
- that’s an emergency. Call your doctor right away. Don’t wait. These changes often mean the drug can cause death, organ failure, or serious injury if used incorrectly.
But if you see:
- “Consider this information when prescribing”
- “Additional monitoring may be needed”
- “Update your records”
- that’s an informational update. It’s still important, but not an emergency. You might need to adjust your next refill or ask your doctor about alternatives.
What to Do If You’re a Patient
If you’re not a doctor, you still need to act. Here’s how:
- Find your medication’s Medication Guide. Every prescription comes with one. It’s a small paper that explains side effects, how to take it, and what to watch for. The FDA requires it to be written at an 8th-grade reading level. But many patients say it’s still hard to understand. If you don’t have one, ask your pharmacist for a copy.
- Check for changes every time you refill. The FDA says to read the guide “every time you receive a prescription.” That’s because the warnings can change. A drug that was safe last year might have new risks this year.
- Ask your doctor: “Has there been a new safety notice about this drug?” Most doctors don’t read every FDA communication. But they should know if your medicine has a Boxed Warning update. Don’t assume they do.
- Sign up for FDA email alerts. Go to fda.gov/drugs/drug-safety-and-availability and scroll to the bottom. You can choose to get alerts only for your specific drug or for your drug class (like “opioids” or “diabetes meds”). It’s free, and it’s the fastest way to know when something changes.
Why Some Safety Warnings Come Too Late
Here’s the hard truth: many serious drug risks aren’t caught until years after the drug is sold. A 2020 study found that, on average, it takes over four years for the FDA to issue a major safety update after the first warning signs appear.
Why? Because rare side effects only show up when a drug is used by hundreds of thousands of people. Clinical trials involve a few thousand patients at most. That’s not enough to catch something that happens in 1 out of 10,000 users.
That’s why FDA safety communications matter. They’re the system that fills that gap. But they’re not perfect. Some patients get confused between a “Drug Alert” (a quick notice) and a full “Drug Safety Communication” (a detailed review). One survey found that 63% of patients thought even minor alerts meant they had to stop their medicine right away.
What’s New in 2026
The FDA is trying to fix these problems. Since 2023, they’ve started releasing plain-language summaries for the most serious safety updates - in both English and Spanish. They’re also testing ways to send alerts directly to patient portals linked to electronic health records. By 2025, you might get a pop-up on your MyChart or Epic account if your drug has a new warning.
They’re also working to improve patient understanding. Right now, only 54% of patients fully understand what a safety communication means. Their goal? Get that to 75% by 2027.
What to Do If You’re Still Confused
If you read a safety communication and feel lost, you’re not alone. Even many pharmacists say the language can be dense.
Here’s what to do:
- Take the document to your pharmacist. They’re trained to read these and can explain what it means for your specific case.
- Search for “FDA [drug name] safety communication summary” on Google. Sometimes patient advocacy groups or medical blogs break it down in plain English.
- Call the FDA’s Drug Information Line at 1-888-INFO-FDA (1-888-463-6332). They can help you find the right document and explain it.
Don’t guess. Don’t ignore it. Don’t assume your doctor already knows. If a safety communication exists for your drug, it’s there for a reason - and you deserve to understand it.
Are FDA safety communications only for doctors?
No. While they include technical details for healthcare providers, every FDA safety communication has a dedicated "For Patients" section written in plain language. You should read this part every time you refill your prescription. These updates can affect whether you should keep taking your medicine, change your dose, or talk to your doctor about alternatives.
What’s the difference between a Drug Alert and a Drug Safety Communication?
A Drug Alert is a short, urgent notice - often just a paragraph - about a serious, immediate risk. A Drug Safety Communication is a full, detailed report that includes background data, labeling changes, and recommendations. Alerts are rare and usually mean you need to act fast. Safety Communications are more common and give you a full picture of what changed and why.
Can I trust the FDA’s safety warnings?
Yes. The FDA bases these warnings on real-world data from doctors, patients, and scientific studies - not just lab results. They review reports from the MedWatch system, clinical trials, and global safety databases. While delays can happen, the process is transparent and evidence-based. If you see a Boxed Warning, it’s been reviewed by multiple experts.
Do all medications have safety communications?
No. Only drugs that have been on the market long enough to reveal new safety issues get these updates. New drugs may have warnings on their labels from the start, but safety communications happen after real-world use. Most brand-name drugs will have at least one safety communication during their lifetime. Generic drugs usually inherit the same warnings as their brand-name counterparts.
What should I do if my drug has a new safety warning?
Don’t stop taking it unless the communication says "STOP." Call your doctor or pharmacist. Ask: "What does this mean for me?" and "Should I change anything?" Many updates just mean you need more monitoring, not a new drug. Never make a decision based on fear - make it based on information.




Jessie Ann Lambrecht
January 7, 2026 AT 00:12Just read this after my pharmacist handed me a new script for my blood pressure med. I didn’t even know these existed. I’m signing up for the email alerts today - no more guessing. This is the kind of info that saves lives, not just paperwork.
Aparna karwande
January 8, 2026 AT 02:11How can you trust an agency that let OxyContin flood the country for a decade before finally admitting it was a nightmare? FDA communications are just PR spin with a fancy logo. They don’t fix systemic corruption - they just make you feel better about swallowing poison while they collect their paycheck.
Vince Nairn
January 10, 2026 AT 00:55Yeah but honestly the FDA is the least worst option we’ve got. I’ve seen pharma companies bury data for years. At least the FDA has a paper trail and a public database. I’m not saying it’s perfect - just that if you’re waiting for Big Pharma to self-regulate, you’re gonna be waiting forever.
Kyle King
January 11, 2026 AT 22:54Wait so you really think the FDA isn’t just a puppet for Big Pharma? I’ve got friends who got liver failure on a drug that had 17 internal warnings buried in the FDA’s own system before they issued a 'safety communication'. They waited 5 years. That’s not transparency - that’s a death sentence with a footnote.
Emma Addison Thomas
January 13, 2026 AT 12:55I’ve been reading these for years since I moved to the States. Back home in the UK, we get similar updates from the MHRA - but they’re always bundled with plain-language leaflets. The FDA’s 'For Patients' section is good, but it still feels like you need a degree to parse it. Maybe they should partner with libraries for community workshops?
Mina Murray
January 15, 2026 AT 01:50Why are you all acting like this is new info? Every single drug has a hidden death clause buried in the fine print. I’ve been tracking this since 2015. The FDA doesn’t warn you - they wait until someone dies in 3 states before they 'update the boxed warning'. And don’t even get me started on how they bury the real stats in PDFs no one reads.
Rachel Steward
January 16, 2026 AT 21:40Let’s be real - this entire system is a performance art piece designed to make you feel safe while the machine keeps grinding. The FDA doesn’t protect patients - it protects the profit margins of companies that pay for their funding. That 'Boxed Warning'? It’s not a red flag. It’s a yellow flag with a lawsuit disclaimer stitched to it. You think they’d ban a drug that kills 1 in 10,000? No. They just add a 200-word paragraph in 8-point font and call it 'transparency'.
And the 'For Patients' section? It’s written by a PR intern who’s never taken a pill in their life. 'Talk to your doctor' - yeah, because that’s always the answer, isn’t it? Meanwhile, your doctor’s got 7 minutes between patients and a 40-page drug guide they’ve never opened.
This isn’t safety. It’s damage control with a smiley face.
Jonathan Larson
January 18, 2026 AT 15:47While the criticisms raised are not without merit, it is important to recognize that post-market surveillance of pharmaceuticals is an inherently complex and statistically challenging endeavor. The FDA operates under constrained resources, and the detection of rare adverse events requires aggregation of data across millions of patients - a process that inevitably involves temporal lag. That said, the recent initiatives toward plain-language summaries and EHR-integrated alerts represent a commendable evolution in patient-centered communication. The goal, as articulated, is not perfection, but progressive improvement.
Katrina Morris
January 20, 2026 AT 08:49i just learned about this today and im so glad i did. i always thought the med guide was just fluff. now i check it every time i get a refill. my mom had a bad reaction last year and we never knew it was on the list. this is life changing info. thank you for sharing
LALITA KUDIYA
January 21, 2026 AT 02:26so true! i read these now and show my uncle who takes 7 meds. he says 'why no one tell me this?' 😔
Christine Joy Chicano
January 22, 2026 AT 03:02There’s a fascinating cognitive dissonance here: we demand transparency from institutions while simultaneously refusing to engage with the complexity of their output. The FDA’s communications are dense because the science is dense. Simplifying too much risks misinterpretation - which is why 'Talk to your doctor' isn’t a cop-out, it’s a necessary safeguard. The real failure isn’t the FDA - it’s our collective refusal to invest time in understanding our own health.
Adam Gainski
January 23, 2026 AT 12:17I work in a clinic and I’ve started printing out the 'For Patients' section and handing it out with scripts. Patients are way more engaged when they can hold it. Also - the email alerts? Game changer. I’ve had two people come in because they got one and were worried. One caught a dangerous interaction before it happened. Small steps matter.
Anastasia Novak
January 24, 2026 AT 02:30Let’s be honest - if you’re reading this and not screaming into the void, you’re not paying attention. The FDA is a bureaucratic graveyard for real accountability. They don’t want you to understand - they want you to feel like you’re being cared for while they quietly approve the next blockbuster that’ll kill 0.01% of users. And guess who pays? You. Your insurance. Your dignity. Your family’s savings.
Alex Danner
January 25, 2026 AT 20:24My dad’s on warfarin. He got the safety update about a new interaction with turmeric supplements. He called his pharmacist, they adjusted his dose, and he’s fine. This system works - not perfectly, but better than it used to. If you’re mad about delays, channel that energy into advocating for better funding for post-market surveillance. Don’t just rant - make it better.