When someone has type 2 diabetes and obesity, losing weight isn’t just about fitting into clothes or looking better. It’s about survival. The body’s ability to use insulin breaks down, blood sugar climbs, and complications like nerve damage, kidney failure, and heart disease start creeping in. For many, diet and pills just don’t cut it anymore. That’s where metabolic surgery comes in-not as a last resort, but as one of the most powerful tools we have to reverse diabetes and reclaim health.
What Metabolic Surgery Actually Does
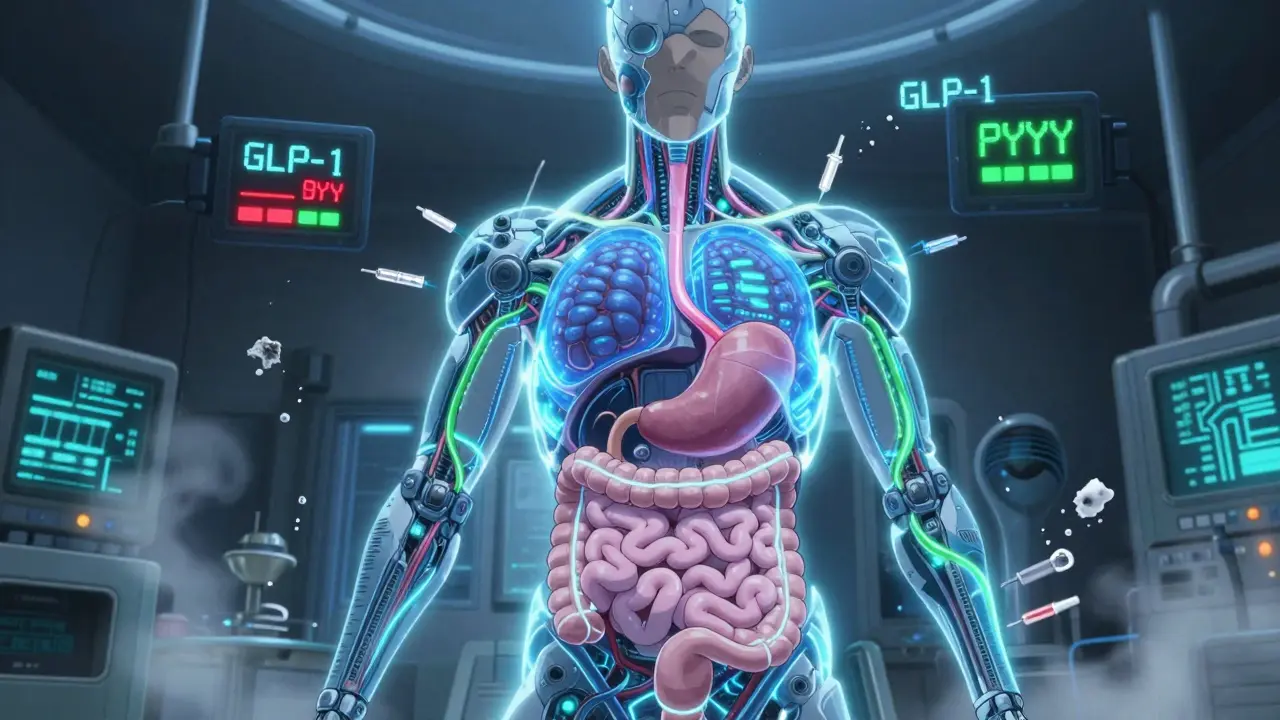
Metabolic surgery, often called bariatric surgery, isn’t just about shrinking your stomach. It’s about rewiring how your body processes food, hormones, and energy. Procedures like gastric bypass, sleeve gastrectomy, and duodenal switch change the anatomy of your digestive tract. That triggers chemical signals from your gut that tell your pancreas to make more insulin, your liver to store less fat, and your brain to feel full faster. The result? Blood sugar drops-even before you lose much weight.Studies show that within days of gastric bypass, many patients see their blood sugar normalize. One patient described it like flipping a switch: "I stopped taking insulin on day three. I didn’t even realize I hadn’t checked my sugar all week." This isn’t magic. It’s biology. The gut hormones GLP-1 and PYY surge after surgery, improving insulin sensitivity and reducing hunger. These changes stick around long after the initial weight loss.
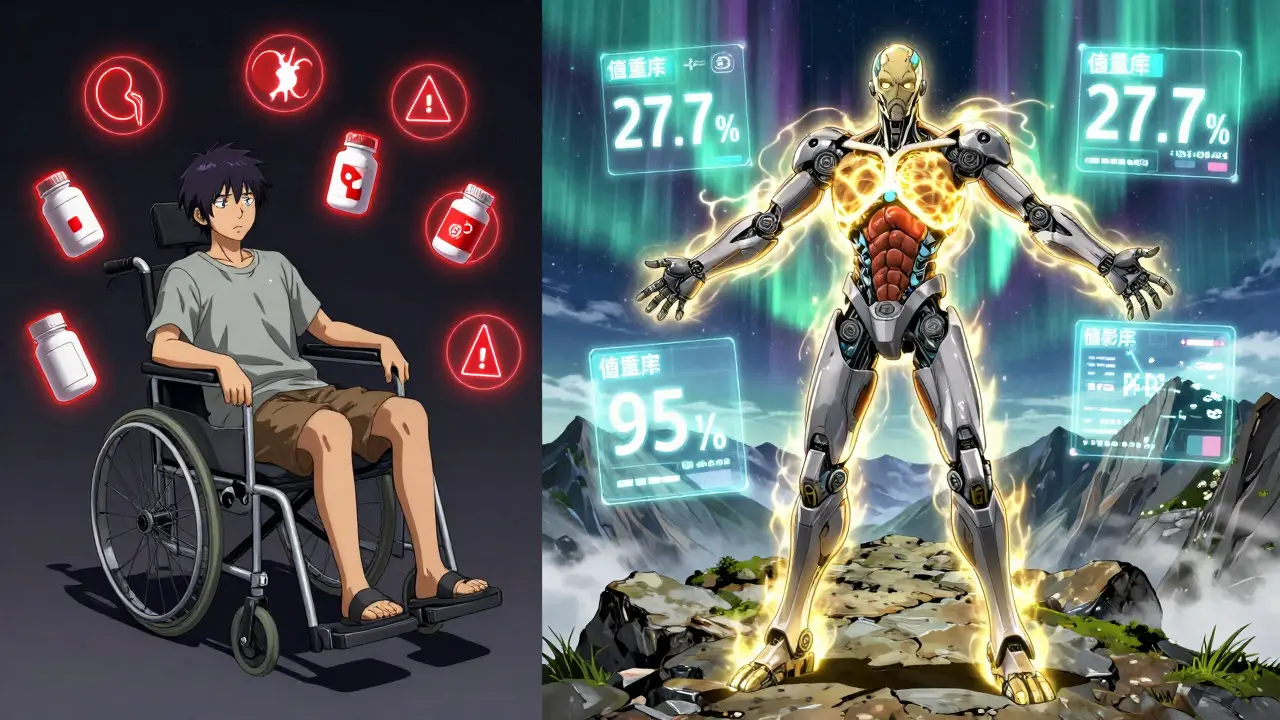
Weight Loss Numbers That Matter
The average person who undergoes metabolic surgery loses about 27.7% of their starting body weight. Compare that to medical therapy alone, where patients lose just 0.2%. That’s not a small difference-it’s life-changing.Take gastric bypass: patients with a BMI of 45.9 lost nearly 20% of their total body weight six years after surgery. Sleeve gastrectomy patients lost about 17% over the same period. Even more striking: those who had biliopancreatic diversion with duodenal switch lost over 30% of their weight on average. These aren’t theoretical numbers. These are real people who went from struggling to walk up stairs to hiking, playing with grandchildren, or returning to work.
But weight loss isn’t the whole story. The real win is what happens to your diabetes.
Diabetes Remission: The Real Goal
Remission doesn’t mean you’re cured. It means your blood sugar is normal without any diabetes medications. And metabolic surgery delivers that more than anything else.One year after gastric bypass, 42% of patients are in full remission. At five years, that number is still at 29%. Sleeve gastrectomy? 37% remission at one year, 23% at five. Even more impressive: patients who had duodenal switch saw remission rates as high as 95% in the first year.
But here’s what most people don’t know: surgery works even for people who aren’t severely obese. A 2019 study looked at patients with a BMI under 30-considered normal or overweight by standard charts. Among them, 93% of gastric bypass patients achieved diabetes remission within a year. That’s a game-changer. It means metabolic surgery isn’t just for the morbidly obese. It’s for anyone with type 2 diabetes who hasn’t responded to other treatments.
Who Benefits Most?
Not everyone responds the same. The data shows clear patterns.- If you’re not using insulin before surgery, your chance of remission jumps to over 50%. Insulin users have lower success rates.
- The lower your BMI before surgery, the better your odds. Patients with BMI 24-30 had remission rates nearly double those with BMI over 40.
- Diabetes duration matters. If you’ve had it less than five years, remission is far more likely.
- Younger patients tend to do better, but age alone isn’t a barrier. Even those in their 60s and 70s see major improvements.
These aren’t random trends. They’re clues. They tell us that metabolic surgery works best when the pancreas still has some function left. Once beta cells are worn out from years of overwork, recovery becomes harder. That’s why early intervention matters.
What Happens After the Surgery?
Surgery isn’t the finish line-it’s the starting line. Long-term success depends on lifelong habits and medical follow-up.Yes, remission rates drop over time. The Swedish Obese Subjects study found that while 72% of patients were in remission two years after surgery, that number fell to 36% after ten years. Why? Weight regain. Slowing metabolism. Progressive beta-cell decline. It’s not failure-it’s biology.
But here’s the key: even when remission fades, most patients still have better blood sugar control than before surgery. They need fewer medications. Their HbA1c stays lower. Their risk of heart disease, kidney damage, and vision loss drops by up to 19% for every year they maintain remission.
And there are risks. Nutritional deficiencies-like iron, B12, calcium, and vitamin D-are common. Bone fractures increase slightly over time. Gastrointestinal issues like dumping syndrome or ulcers can occur. That’s why every patient needs a team: a surgeon, a dietitian, an endocrinologist, and a mental health provider. Regular blood tests aren’t optional. They’re essential.
How It Compares to Other Treatments
The ARMMS-T2D trial compared surgery to intensive medical therapy over seven years. Surgery led to 18.2% diabetes remission. Medical therapy? Just 6.2%. That’s a three-fold difference.Even the best non-surgical options fall short. The DiRECT trial showed that a very low-calorie diet could get 46% of patients into remission at one year. Sounds good, right? But after five years, most of those people gained the weight back-and so did their diabetes. Surgery doesn’t have that same rebound effect. The metabolic changes stick.
And it’s not just about sugar. Surgery improves cholesterol, triglycerides, and blood pressure. HDL (good cholesterol) goes up. Triglycerides drop by 40% or more. These are the hidden drivers of heart disease-and surgery tackles them head-on.
Why Isn’t Everyone Getting It?
Despite the evidence, only 1-2% of eligible patients in the U.S. get metabolic surgery each year. Why?- Insurance won’t cover it if your BMI is under 35-even if you’re insulin-dependent and your A1c is 9.5.
- Doctors don’t talk about it. Many still think of bariatric surgery as a "cosmetic" fix for obesity, not a treatment for diabetes.
- Patients fear surgery. They hear "gastric bypass" and think "risky." But complication rates are now lower than gallbladder removal.
- There’s a myth that you’ll regain all the weight. But studies show most patients keep off 50-70% of lost weight after ten years.
The truth? We’re underusing a tool that saves lives. The American Diabetes Association has endorsed metabolic surgery since 2016. The International Diabetes Federation did the same in 2011. The science is settled. The barrier isn’t evidence-it’s access.
What’s Next for Metabolic Surgery?
New, less invasive options are emerging. Endoscopic procedures like intragastric balloons and aspiration systems offer middle-ground solutions for people who aren’t ready for full surgery. The RESET trial is testing whether surgery should be approved for people with BMI as low as 27. That could open the door to millions more.But the biggest shift isn’t in the operating room. It’s in how we think. Metabolic surgery isn’t a quick fix. It’s a lifelong reset. It requires commitment, support, and ongoing care. But for those who qualify, it’s the closest thing we have to a cure for type 2 diabetes.
If you or someone you know has type 2 diabetes and struggles with weight, ask this: What’s the cost of waiting? Every year without intervention means more damage to your organs, more pills, more doctor visits, more risk. Surgery isn’t the easy path-but for many, it’s the only path that leads to real freedom.
Can metabolic surgery cure type 2 diabetes?
Metabolic surgery doesn’t guarantee a permanent cure, but it can lead to long-term remission-meaning normal blood sugar without medication. About 30% of patients remain in remission 15 years after surgery. Even when diabetes returns, most people still have better control and need fewer drugs than before.
Is metabolic surgery only for people with severe obesity?
No. While surgery is often recommended for BMI 35 or higher, studies show it works well for people with BMI as low as 27. In fact, patients with lower BMI often have higher remission rates. Guidelines now support surgery for those with type 2 diabetes and BMI 30-34.9 if medications aren’t working.
How soon after surgery does diabetes improve?
Many patients see blood sugar drop within days-even before losing significant weight. This is because surgery changes gut hormones that regulate insulin. Some stop insulin or oral meds within the first week. The faster the improvement, the better the long-term outlook.
What are the biggest risks of metabolic surgery?
The most common long-term risks are nutritional deficiencies-especially in iron, B12, calcium, and vitamin D. Other risks include gastrointestinal issues like dumping syndrome, ulcers, and a slightly higher chance of bone fractures. These are manageable with regular blood tests, supplements, and follow-up care. Serious complications like leaks or infections are rare-less than 2% in experienced centers.
Will I need to take supplements for the rest of my life?
Yes. After most metabolic surgeries, your body absorbs fewer nutrients. Lifelong daily supplements are required: a multivitamin, calcium, vitamin D, and often iron and B12 injections or high-dose pills. Skipping them can lead to anemia, nerve damage, or osteoporosis. This isn’t optional-it’s part of the treatment.
Can I have metabolic surgery if I’m on insulin?
Yes, but remission rates are lower than for non-insulin users. About 30-40% of insulin users still achieve remission after surgery, compared to over 50% for those not on insulin. The key is timing: the sooner you act after starting insulin, the better your chances. Delaying surgery reduces the likelihood of reversing diabetes.
Is metabolic surgery covered by insurance?
Coverage varies. Most insurers cover surgery for BMI 35 or higher with diabetes. For BMI 30-34.9, coverage is inconsistent and often requires proof that medications failed. Some states mandate coverage for metabolic surgery in diabetes patients regardless of BMI. Always check your plan and ask for a predetermination letter.
How do I know if I’m a candidate?
You’re likely a candidate if you have type 2 diabetes and a BMI of 30 or higher, especially if you’re on medication and your A1c is above 7.5%. You should have tried at least six months of lifestyle changes and medications without success. A multidisciplinary team-including a surgeon, dietitian, and psychologist-will evaluate your medical history, mental health, and readiness for lifelong changes.



Mike Rengifo
December 17, 2025 AT 19:44Been following this thread and just wanted to say - I had the sleeve last year. Lost 80 lbs. Stopped metformin by week 2. My A1c’s been 5.1 for 11 months now. No magic. Just biology. And yeah, I take my B12 like it’s my job now. But honestly? Worth every second of the nausea and the weird food aversions.
Meenakshi Jaiswal
December 19, 2025 AT 12:21For anyone considering this - talk to a dietitian BEFORE surgery. Not after. The prep matters more than you think. And don’t wait until you’re on insulin. The sooner you act, the better your odds. I’ve seen too many people regret delaying.
Ashley Bliss
December 21, 2025 AT 02:32This is what happens when you let corporations decide what ‘health’ means. They don’t want you cured - they want you on meds forever. Surgery? Too permanent. Too cheap. Too real. The pharmaceutical industry is terrified of this. That’s why your doctor won’t mention it. That’s why insurance fights it. This isn’t medicine. It’s a profit model.
They’ll tell you it’s risky. But what’s riskier? Dying of a heart attack at 52? Or losing 30% of your weight and walking your daughter down the aisle? They don’t want you to ask that question.
They’ll say ‘lifestyle changes.’ But if diet and exercise worked, why are we drowning in diabetic amputations? Why are kids getting type 2 now? This isn’t about willpower. It’s about broken biology. And the system doesn’t profit from fixing it.
I lost my dad to diabetes complications. He was told to ‘eat less sugar.’ He did. He lost 50 pounds. Still died. Because they never told him about surgery. They told him to take more pills.
They call this ‘bariatric.’ Like it’s about looks. It’s not. It’s about survival. And if you’re not advocating for this for everyone who needs it - you’re part of the problem.
They’re not denying care. They’re denying access. And that’s not an oversight. It’s policy.
And don’t get me started on how they market this as ‘cosmetic’ while charging $30k out of pocket. Meanwhile, a year of Ozempic costs $15k and doesn’t fix anything. Just delays the inevitable.
Wake up. This is a human rights issue. Not a medical one.
pascal pantel
December 22, 2025 AT 14:17Let’s be real - the 95% remission rate for duodenal switch is cherry-picked from a cohort of patients with BMI <35 and diabetes duration <3 years. The real-world numbers? More like 58%. And the long-term complication profile? Unacceptable. Malnutrition, osteoporosis, protein deficiency - these aren’t side effects. They’re systemic consequences of altering gut anatomy for a chronic condition that should be managed pharmacologically.
Also, the ARMMS-T2D trial had a 12% dropout rate. That’s not insignificant. And the ‘remission’ definition? Fasting glucose <126. That’s not a cure. That’s a lab result. You’re still metabolically compromised. The beta cells are still exhausted. You’re just masking it with altered physiology.
And don’t get me started on the ethics of pushing surgery on low-BMI patients. We’re medicalizing normal human variation. This is the new frontier of pathologizing fat. It’s not science. It’s neoliberal biocontrol.
Dev Sawner
December 23, 2025 AT 11:54While the data presented is statistically significant, one must consider the selection bias inherent in surgical cohorts. Patients who undergo metabolic surgery are typically highly motivated, possess higher socioeconomic status, and have access to multidisciplinary follow-up - factors that independently correlate with improved outcomes. The comparative studies often fail to control for these confounders.
Furthermore, the definition of 'remission' is inconsistent across studies. Some use HbA1c thresholds, others fasting glucose, and some include medication cessation without longitudinal follow-up. This renders meta-analyses unreliable.
It is also noteworthy that the long-term data from the Swedish Obese Subjects study, while robust, is observational and non-randomized. The control group received standard care, which in Sweden in the 1990s was markedly different from contemporary U.S. protocols.
Thus, while the results are encouraging, they should not be extrapolated to the general diabetic population without rigorous RCTs controlling for psychosocial and economic variables.
Anna Sedervay
December 24, 2025 AT 10:05It’s fascinating how the medical establishment has suddenly embraced surgery as a ‘solution’ - as if the body’s natural regulatory systems are inherently flawed, rather than the result of decades of industrialized food policy, sedentary labor, and corporate manipulation of nutrient profiles. We’ve pathologized survival mechanisms. We’ve turned adaptation into disease.
And yet - no one dares mention the elephant in the room: the FDA approved GLP-1 agonists after 18 months of trials. But metabolic surgery? Requires a decade of longitudinal data. Why? Because it’s not patentable. It’s not profitable. It’s a public health intervention disguised as a surgical procedure.
They’ll give you Ozempic for $15,000 a year. But ask for gastric bypass? ‘We’ll need a 12-week psychological evaluation, proof of 6 months of dieting, and a letter from your pastor.’
It’s not about safety. It’s about control. And if you’re not seeing that - you’re being manipulated.
Sahil jassy
December 25, 2025 AT 21:04Kathryn Featherstone
December 26, 2025 AT 04:25I’m a nurse who works in endocrinology. I’ve seen patients cry after their first sugar-free week. I’ve seen grandparents play with grandkids again. I’ve also seen the ones who skip their vitamins and end up in the ER with neuropathy. This isn’t a quick fix - it’s a lifestyle overhaul. But for the right person? It’s the best gift medicine has ever given.
Just don’t go in thinking it’s easy. It’s not. But it’s worth it.
bhushan telavane
December 27, 2025 AT 05:24In India, this is still a luxury. Most people can’t even afford insulin, let alone surgery. But I’ve seen rural patients travel 800km for this - and come back with their lives back. The cost is high, yes. But the cost of doing nothing? Higher. We need government subsidies. Not just for the rich.
Dikshita Mehta
December 28, 2025 AT 01:35One thing everyone misses: the psychological impact. Many patients report feeling ‘free’ for the first time - not just from sugar, but from shame. The weight wasn’t the problem. The stigma was. Surgery doesn’t erase that, but it gives you space to heal from it. That’s not in the studies. But it’s real.
Matt Davies
December 29, 2025 AT 11:55Man, this is the closest thing we’ve got to a diabetes reset button. I mean - imagine flipping a switch and your body just… remembers how to work. No more midnight glucose checks. No more counting carbs like you’re doing calculus. Just… normal. I’ve got a cousin who went from wheeling a walker to hiking Machu Picchu. That’s not medicine. That’s liberation.
Yeah, you gotta take supplements. Yeah, you gotta chew slow. Yeah, you can’t eat a whole pizza anymore. But you can eat ice cream without panic. You can eat birthday cake without guilt. You can live.
And honestly? If this was a pill, it’d be the most expensive drug on the planet. But because it’s surgery? They treat it like a last-resort gamble. What a crock.
Sajith Shams
December 29, 2025 AT 21:33The data is manipulated. You cite remission rates but ignore the fact that 40% of patients develop bile reflux, 22% develop anemia severe enough to require transfusions, and 18% report chronic nausea that persists beyond two years. The mortality rate is low - yes - but morbidity? Catastrophic. And the ‘weight loss’? Mostly fluid and muscle. Fat loss is minimal in many cases. You’re trading one chronic condition for three others.
And let’s not pretend this isn’t a profit machine for hospitals. The average reimbursement for gastric bypass is $28,000. The cost of care? $6,000. That’s a 366% markup. This isn’t healing. It’s a business model.
mary lizardo
December 30, 2025 AT 01:06It is patently irresponsible to promote invasive, irreversible surgical interventions as a first-line treatment for a metabolic condition that is, in nearly all cases, rooted in behavioral and environmental factors. To suggest that anatomy is the primary determinant of insulin resistance is a gross oversimplification - one that absolves individuals of personal responsibility and diverts resources from public health initiatives that could address the root causes: ultra-processed food systems, food deserts, and sedentary urban design.
Furthermore, the normalization of surgical intervention for BMI 30 undermines decades of medical ethics regarding bodily autonomy and the principle of non-maleficence. We are not merely repairing malfunctioning organs - we are reshaping human physiology to conform to aesthetic and economic norms disguised as medical necessity.
The American Diabetes Association’s endorsement is not evidence of scientific consensus - it is evidence of institutional capture by surgical interest groups.
Moses Odumbe
December 31, 2025 AT 11:02Bro. I got the sleeve. Lost 102 lbs. Stopped metformin. My wife says I’m ‘lighter’ - literally and emotionally. 😊 But yeah - I take B12 shots every week. Like clockwork. And I can’t have bread anymore. But I can run 5K. So… worth it. 🤷♂️
Sahil jassy
January 1, 2026 AT 08:36My cousin got the bypass last year. Same story - no insulin in 7 days. But now she’s got chronic diarrhea. And her hair’s falling out. She says it’s worth it. But I worry.
Meenakshi Jaiswal
January 1, 2026 AT 21:45That’s why follow-up is everything. Diarrhea? Could be bile acid malabsorption - easy to fix with cholestyramine. Hair loss? Usually temporary - caused by rapid weight loss and low protein. Most patients bounce back in 6 months with proper nutrition. The key is staying with your team. Not going silent after the first month.