When you’re managing medications-whether for yourself, a loved one, or as a healthcare provider-knowing what drugs are being taken is only half the battle. The real lifesaver? Documenting safety alerts on your medication list. These aren’t just reminders. They’re critical warnings that stop errors before they happen. Think insulin overdoses, blood thinners causing internal bleeding, or muscle relaxants leading to respiratory arrest. These aren’t rare mistakes. They’re preventable-and documentation is the key.
Why Safety Alerts Matter More Than You Think
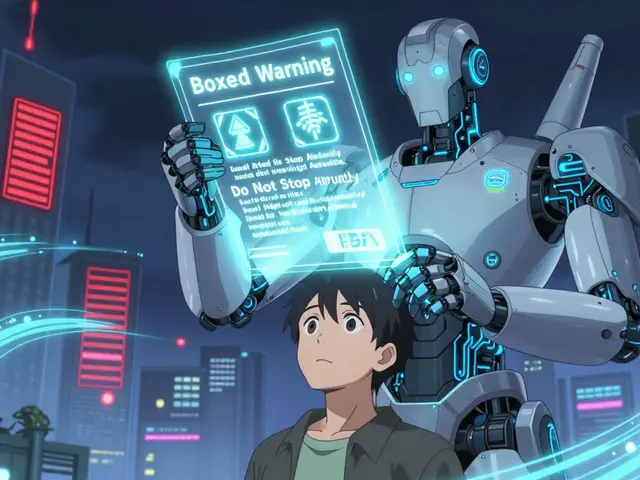
Not all medications are created equal. Some carry what the Institute for Safe Medication Practices (ISMP) calls high-alert medications. These are drugs that, when used incorrectly, can cause serious harm or death. The current ISMP list includes 19 categories: insulin, opioids, anticoagulants, neuromuscular blockers, chemotherapy agents, and more. According to the World Health Organization, properly documented safety alerts can cut medication errors by up to 50% in hospitals. That’s not a guess. It’s backed by data from over 150 healthcare facilities.But here’s the catch: a warning on a pill bottle isn’t enough. An alert in an electronic system that gets ignored? That’s worse than nothing. Real safety comes from documentation that links the alert to a clear action. For example, if someone is on oral methotrexate (a chemotherapy drug), the system should force the prescriber to document the correct cancer diagnosis before the order goes through. It shouldn’t just say "Check dose." It should demand proof.
What Exactly to Document
You’re not just writing notes. You’re building a safety system. Here’s what needs to be documented for each high-alert medication:- Drug name and strength - Not just "insulin," but "U-100 regular insulin 10 units subcutaneous."
- Reason for use - Why is this drug being given? "For Type 2 diabetes" is too vague. "For hyperglycemia with HbA1c of 9.2%" is specific.
- Alert label - Use exact wording from official guidelines. For neuromuscular blockers, the label must say: "WARNING: CAUSES RESPIRATORY ARREST - PATIENT MUST BE VENTILATED." No shortcuts.
- Verification steps taken - Did you double-check the dose? Was barcode scanning used? Was a second clinician present? Record it.
- Patient education confirmation - Did the patient understand how to take it? Did they know the signs of overdose? Document their understanding.
These aren’t optional. The Joint Commission requires this documentation for accredited hospitals. And starting in 2025, Medicare will tie reimbursement to whether these records are complete and accurate.

How to Set Up Your Documentation System
Whether you’re a hospital, clinic, or someone managing meds at home, you need structure. Here’s how to build it:- Identify your high-alert medications - Start with the ISMP 2024-2025 list. Tailor it to your setting. A rural clinic won’t use the same drugs as a trauma center.
- Choose your format - Paper? Electronic? Hybrid? Electronic systems with built-in alerts are best. But if you’re using paper, create a standardized form with checkboxes for each safety step.
- Integrate alerts into workflows - Don’t add alerts as an afterthought. Make them part of prescribing, dispensing, and administering. For example, if a nurse skips scanning a barcode, the system should pause and require a reason.
- Track compliance - Monitor how often alerts are bypassed. If more than 5% of alerts are ignored, dig into why. Is it confusion? Lack of training? System glitches?
- Review monthly - Have a safety team meet every month. Look at near-misses. Celebrate wins. Fix gaps. This isn’t a one-time project. It’s ongoing.
One hospital in Ohio cut its insulin errors by 71% in just 14 months by doing exactly this. They didn’t buy fancy software. They just made sure every step was documented and reviewed.
Common Mistakes to Avoid
Even good systems fail when people cut corners. Here are the biggest pitfalls:- Too many alerts - If every medication triggers five pop-ups, clinicians start ignoring them. The goal isn’t to warn about everything. It’s to warn about what matters. Studies show systems with more than 15 alerts per order have a 69% bypass rate.
- No follow-up - Documenting an alert without acting on it is pointless. If you note that a patient is on warfarin, you must also document INR levels, diet changes, and drug interactions checked.
- Using vague language - "Use caution" or "Monitor closely" means nothing. Be specific: "Check INR weekly. Hold dose if INR > 5.0. Avoid NSAIDs."
- Ignoring external alerts - The FDA releases about 120 drug safety notices every year. If your system doesn’t have a way to absorb these into your documentation, you’re flying blind.

Real-World Success and Struggles
Pharmacists at the University of Michigan reported a 63% drop in high-alert medication errors after implementing full documentation. But they also had to hire a dedicated staff member just to manage the paperwork. That’s the trade-off.On the flip side, rural clinics struggle. One nurse on Reddit wrote: "We’re supposed to document every bypassed alert. But with 3 pharmacists covering 24/7? We don’t have time. It feels like box-checking." That’s the reality for many. The solution isn’t to give up. It’s to simplify. Start with just two or three high-alert drugs. Master those. Then expand.
AI is coming. Epic Systems is rolling out a tool in mid-2025 that automatically prioritizes alerts based on your facility’s error history. But early versions had an 18% false-negative rate-meaning they missed real dangers. So even with tech, human oversight is still essential.
What’s Next for Medication Safety
The future is automated-but not fully. By 2027, the ECRI Institute predicts 75% of U.S. hospitals will use AI to auto-document safety alerts, reducing errors by another 22%. But the core won’t change: documentation must be tied to action.Right now, the FDA’s Sentinel Initiative is making it easier. It sends automated safety alerts directly into hospital systems, cutting manual entry by 80%. That’s huge. But if your documentation process doesn’t respond to those alerts with clear actions, you’re still at risk.
Medication safety isn’t about having the most alerts. It’s about having the right ones-and making sure every alert leads to a documented, verified step that protects the patient.
What are high-alert medications?
High-alert medications are drugs that carry a higher risk of causing serious harm if used incorrectly. Examples include insulin, opioids, anticoagulants like warfarin, neuromuscular blockers, and chemotherapy agents. The Institute for Safe Medication Practices (ISMP) maintains the official list, which currently includes 19 categories. These drugs require extra documentation and verification steps to prevent errors.
Do I need to document safety alerts if I’m managing meds at home?
Yes. Even at home, documenting alerts saves lives. For example, if you take warfarin, note your latest INR number, any new medications you started, and whether you changed your diet (like eating more leafy greens). Write it on a sheet of paper, use a phone app, or sync it with your pharmacy’s portal. The goal is to make sure anyone who helps you-family, nurse, ER doctor-sees the full picture.
How often should I review my medication safety documentation?
Review it every time your meds change-and at least once a month. If you’re on a high-alert drug like insulin or blood thinners, check your documentation weekly. Look for gaps: Did you forget to note a new drug interaction? Did your dose change without updating the record? Regular reviews turn documentation from a chore into a safety net.
Can electronic health records (EHRs) handle this automatically?
EHRs can help, but they don’t replace good documentation. Many systems trigger alerts, but clinicians often bypass them if they’re too frequent or unclear. The best EHRs include hard-stop prompts that require you to enter a reason before proceeding. Look for systems that link alerts to required fields-like forcing you to document an INR value before approving a warfarin refill.
What if my pharmacy or doctor ignores my safety alerts?
Take control. Print your documented safety alerts and bring them to every appointment. Ask: "Did you see this alert?" If they say no, request that it be added to their system. You are your own best advocate. If you’re on insulin or a blood thinner, don’t rely on someone else to remember. Your documentation is your shield.