Getting your prescription filled should be simple. But what if the label says someone else’s name? Or the pill looks different from what your doctor described? These aren’t just rare mistakes-they happen more often than you think. In fact, prescription label errors are behind nearly one in four preventable medication mistakes, according to the Institute for Safe Medication Practices. That’s why checking your label before leaving the pharmacy isn’t optional-it’s your last line of defense.
Why Checking Your Prescription Label Matters
Every year, over 1.5 million people in the U.S. experience medication errors. Many of these happen because the label doesn’t match what was prescribed. You might get the right pill but the wrong dose. Or your name might be printed on someone else’s bottle. These aren’t just mix-ups-they can cause serious harm, even death. The good news? You don’t need to be a pharmacist to catch these mistakes. A simple 30-second check can prevent a dangerous error. Studies show that when patients verify their prescriptions, the chance of taking the wrong medication drops by 67%. That’s not a small boost-it’s life-saving.What Should Be on Your Prescription Label
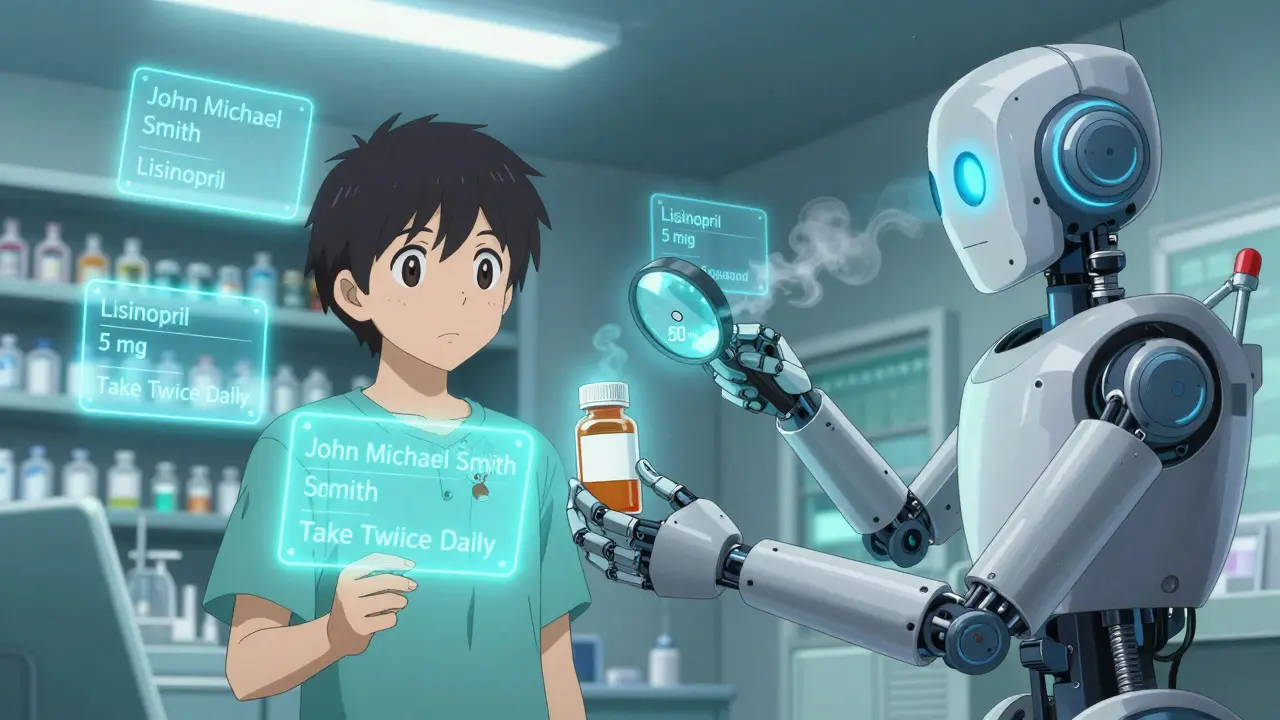
By law, every prescription label must include six key pieces of information. If any are missing or unclear, ask the pharmacist before you leave.- Your full legal name (first and last, sometimes middle initial)
- The medication name (both brand and generic, like “Lisinopril” and “Zestril”)
- The strength (e.g., “5 mg,” “10 mg”-never assume)
- The dosage instructions (e.g., “Take one tablet by mouth twice daily”)
- The pharmacy’s name and phone number
- The prescription number and date filled
Step-by-Step: How to Verify Your Label
Follow these six steps every time you pick up a prescription. It takes less than a minute, and it’s worth it.- Hold the bottle at eye level. Make sure you’re in good lighting-natural light or a bright lamp works best. Poor lighting is one reason people miss errors.
- Check your name. Does it match exactly what you gave the pharmacy? No nicknames. No missing middle names. If it says “J. Smith” but you’re “John Michael Smith,” ask about it.
- Match the medication name. Compare the label to what your doctor told you. If they said “blood pressure pill,” but the label says “Lisinopril,” that’s fine-but make sure you know the name. Ask if you’re unsure.
- Confirm the strength. This is where most mistakes happen. A 5 mg pill is not the same as a 50 mg pill. Look closely. If the number seems off, hold it up to the light or ask the pharmacist to show you the original prescription.
- Read the directions. Does it say “take once daily” when your doctor said “twice daily”? That’s a red flag. Don’t assume you remember correctly-check the label.
- Check the pharmacy info. The phone number should be legible. If it’s smudged or missing, that’s a sign something went wrong behind the counter.

Common Problems and How to Fix Them
Even when you check carefully, things can still go wrong. Here are the most common issues-and how to handle them.- Small print. Over 37% of people over 65 struggle to read labels. Use a pocket magnifier (2x magnification works well) or your phone’s camera zoom. Most smartphones let you pinch to zoom on the label.
- Similar-sounding names. “Lopressor” and “Lopid” sound alike but treat very different conditions. If two medications look similar, ask the pharmacist to spell them out.
- Wrong pill shape or color. Pills change between refills. That doesn’t mean it’s wrong-but if it looks completely different, ask. Sometimes generic brands switch manufacturers. A quick call to the pharmacy can clear it up.
- Confusing abbreviations. “QD” means once daily. “BID” means twice daily. If you’re unsure, ask the pharmacist to explain in plain language.
What to Do If Something’s Wrong
If you spot an error-don’t take the medication. Don’t just return it. Say this:- “I think there’s a mistake. My name is [your full name], but the label says [different name].”
- “The strength says 50 mg, but my doctor prescribed 5 mg.”
- “The directions say ‘twice daily,’ but my doctor said once.”
When to Ask for Help
You don’t have to do this alone. If you’re unsure, bring someone with you. Or call the pharmacy ahead of time. The American Pharmacists Association offers a free Medication Safety Helpline: 1-800-987-7856. They can help you understand what’s on your label. Also, if you take five or more medications, ask for a medication review. Many pharmacies offer this for free. A pharmacist can map out all your pills, check for interactions, and make sure your labels are clear.
What’s Changing in 2026
By the end of 2025, all U.S. pharmacies must follow a new FDA standard for prescription labels. The biggest change? Your name will be printed in 24-point font-at the top of the label. This makes it impossible to miss. Other improvements include:- Bigger, clearer type for medication names and dosages
- QR codes on labels that link to video instructions in multiple languages
- Standardized layout so labels look the same across all pharmacies
Real Stories: What Happens When People Check
One woman in Texas picked up her mother’s blood thinner and noticed the strength was 10 mg instead of 5 mg. She asked. The pharmacy had accidentally filled the wrong bottle. A simple check saved her mother from a life-threatening overdose. Another man in Florida took his wife’s blood pressure pill by mistake because the label had his name but the pill looked different. He didn’t question it-until he felt dizzy. He went back. The pharmacy had printed his name on her bottle. That kind of error happens more than you think. These aren’t rare. In a 2023 survey, 18% of patients said they found an error on their label in the past year. Most caught it themselves.Final Thought: Your Safety Is Your Responsibility
Pharmacies do their best. But they’re busy. People work fast. Mistakes happen. The system isn’t perfect. That’s why your check matters. You’re not being difficult. You’re being smart. You’re not second-guessing the pharmacist-you’re completing a safety chain that includes your doctor, the pharmacy, and now you. Take 30 seconds. Hold the bottle up. Read the label. Ask one question if something feels off. It’s not just advice. It’s your right.What if my name is misspelled on the prescription label?
If your name is misspelled, do not take the medication. Even a small error like “John” instead of “Jonathan” can mean the bottle was meant for someone else. Return to the pharmacy and ask them to verify the original prescription with your doctor. Most pharmacies will re-label the medication at no cost. This is a common error, especially when names are similar or when prescriptions are processed electronically.
Can I use my phone to read a small prescription label?
Yes. Use your smartphone’s camera and zoom feature to enlarge the text. Most phones have a built-in magnifier tool under Accessibility settings. You can also use apps like Google Lens to capture and read text from the label. This is especially helpful for people with low vision or older adults. However, remember that digital tools supplement-not replace-manual verification. Always confirm the information yourself.
Why does my medication look different this time?
Generic medications often change color, shape, or size between refills because different manufacturers produce them. This doesn’t mean the medication is wrong-just that the pharmacy switched suppliers. Check the name and strength on the label. If those match what your doctor prescribed, it’s safe. If you’re unsure, call the pharmacy. They can tell you which manufacturer made this batch.
What should I do if the directions don’t match what my doctor said?
Never assume you misremembered. If the label says “take twice daily” but your doctor said “once daily,” ask the pharmacist to check the original prescription. This is one of the most common errors. The pharmacy may have misread the doctor’s handwriting or entered the wrong instructions. The pharmacist can call the doctor’s office to confirm. Always get clarification before taking the medication.
Are there tools or resources to help me understand my prescription label?
Yes. The FDA offers a free guide called “How to Read a Prescription Label,” updated in March 2023. Many pharmacies have in-store verification stations with magnifiers and large-print instructions. You can also call the American Pharmacists Association’s Medication Safety Helpline at 1-800-987-7856. They’ll walk you through what’s on your label and explain any confusing terms.
Do all pharmacies have the same label format?
Not yet, but they will by the end of 2025. The FDA is requiring all pharmacies to use a standardized label layout with your name in 24-point font at the top, medication name in large print, and dosage instructions clearly separated. This change is designed to reduce confusion and make errors easier to spot. Until then, labels vary by pharmacy chain and region-but the required information (name, drug, strength, directions) must always be present.



Jim Johnson
February 13, 2026 AT 12:50Just picked up my dad's blood pressure med yesterday and noticed the pill color was off. Didn't say anything at first, thought maybe it was a different generic. Then I checked the name and strength - perfect match. Called the pharmacy anyway. They said yeah, switched manufacturers last week. Gave me a free magnifier too. Seriously, 30 seconds saves lives. Thanks for the reminder.
Luke Trouten
February 14, 2026 AT 14:40It’s fascinating how such a simple act - verifying a label - becomes an act of radical self-advocacy in a system designed for volume, not vigilance. The fact that 67% reduction in errors comes from patient verification speaks volumes about institutional negligence. We’re not asking for perfection; we’re asking for basic dignity. The FDA’s 2026 changes are a step, but they shouldn’t be the ceiling. This should be standard everywhere, not just a reactive fix.
Kristin Jarecki
February 16, 2026 AT 01:35As a former pharmacy technician, I can confirm that mislabeling is often the result of rushed workflows, not negligence. Pharmacies are understaffed, overwhelmed, and under constant audit pressure. That said, patient verification is not an inconvenience - it’s a necessary layer of safety. I always encouraged patients to double-check. One woman caught a 10x dosage error because she noticed the pill count didn’t match her last refill. She saved her own life. Please keep doing this.
Jonathan Noe
February 16, 2026 AT 02:51Okay but let’s be real - if your name is on the label but the pill looks like a neon green tennis ball, you should still question it. I once got a generic version of metformin that looked like it was made in a lab experiment gone wrong. Took it anyway because I trusted the name. Felt like I’d been injected with a glow stick. Turned out it was just a different coating. Still, I called them. They apologized and gave me a $10 gift card. Worth it.
Pat Mun
February 17, 2026 AT 15:38I’m 68 and I’ve been doing this for years. My eyes aren’t what they used to be, so I use my phone’s zoom feature religiously. I also keep a little notebook where I write down the name, strength, and color of every med I get - just in case something changes. Last month, my new refill had a different manufacturer, and the pill was a different shape. I pulled out my notebook, compared it to last time, and called the pharmacy. They said, ‘You’re right - we sent the wrong batch.’ I didn’t take it. They fixed it. That’s how you stay safe. Don’t be shy. You’re not bothering them - you’re helping them do their job better.
Sophia Nelson
February 18, 2026 AT 21:24Why are we putting this burden on patients? Why isn’t the system just fixed? This is a massive liability issue. Someone should be held accountable. Pharmacies are corporations - they’re not charities. If they can’t get this right, they shouldn’t be allowed to dispense medication. I don’t want to be a detective. I want to be a patient. This is ridiculous.
Neha Motiwala
February 20, 2026 AT 11:36Have you ever thought that maybe the label errors are intentional? Like… what if the government is testing how many people actually read their labels before taking pills? What if they’re quietly tracking who’s compliant and who’s not? I read somewhere that the NDC code can be used to trace your movements. And the QR codes? They’re not for instructions - they’re for data harvesting. I don’t trust any of this. I don’t even take pills anymore. I drink chamomile tea now. It’s safer.
Ojus Save
February 21, 2026 AT 13:50good point about the phone zoom thing. i always use that. but sometimes the lighting is bad and the text gets blurry. also sometimes the pharmacy prints the name in tiny font even though the law says it should be big. i dont get it. i just call them. they dont mind. theyre nice. i think.
Jack Havard
February 22, 2026 AT 00:1767% reduction? That number feels cherry-picked. Where’s the peer-reviewed study? Also, ‘life-saving’ is hyperbolic. Most label errors are caught before ingestion. The real problem is that pharmacies are forced to use outdated software. The FDA’s 2026 changes are too little, too late. And don’t get me started on QR codes - they’re a marketing gimmick. I’ve scanned three. Two led to ads. One was broken. I’m not convinced this is progress.
Gloria Ricky
February 22, 2026 AT 02:03my mom used to get confused with her meds all the time. i started going with her to the pharmacy. we’d hold the bottle up to the light and read it out loud. now she does it by herself. she says it makes her feel in control. i think that’s the real win - not just avoiding mistakes, but feeling like you’re not powerless. small checks = big peace of mind.
Stacie Willhite
February 22, 2026 AT 07:21I just want to say thank you to the people who wrote this. I’ve been too scared to speak up at the pharmacy before. I thought I’d sound dumb. But reading this made me realize - I’m not being difficult. I’m being careful. I’m going to try this next time I pick up my insulin. I’ve got a little notebook now. I’m going to write everything down. Thank you.
Sonja Stoces
February 24, 2026 AT 00:12Wow, what a performative safety checklist. ‘Hold the bottle at eye level.’ Like we’re all supposed to be doing yoga with our prescriptions. And ‘ask the pharmacist to spell it out’? You think they have time? They’re juggling 12 other customers and a printer jam. This isn’t empowerment - it’s gaslighting. The system’s broken. Stop telling patients to fix it with a magnifier. Fix the damn system.
Gabriella Adams
February 24, 2026 AT 05:31I’ve worked in public health for 18 years. This isn’t just about labels - it’s about health literacy. Many people don’t know what ‘BID’ means. Many don’t know their own medication names. The FDA’s new standards are critical - but they’re only part of the solution. We need community education programs, multilingual labeling, and pharmacist-led consultations. This post is a great start. Let’s turn it into action.
Vamsi Krishna
February 24, 2026 AT 13:14Let me tell you about my cousin’s aunt’s neighbor who got the wrong pill because the pharmacy used a font that was too small. The pill was purple. The label said ‘5mg.’ But the bottle was labeled ‘Lisinopril.’ Turns out, the pharmacist was on a 36-hour shift and had mixed up three prescriptions. The guy ended up in the ER. The pharmacy paid $200K. But they didn’t fire him. They just moved him to night shift. So now, every time I pick up a prescription, I bring a lawyer. Just in case. You think I’m joking? I’m not. This is how the system works.