Medication Reaction Emergency Checker
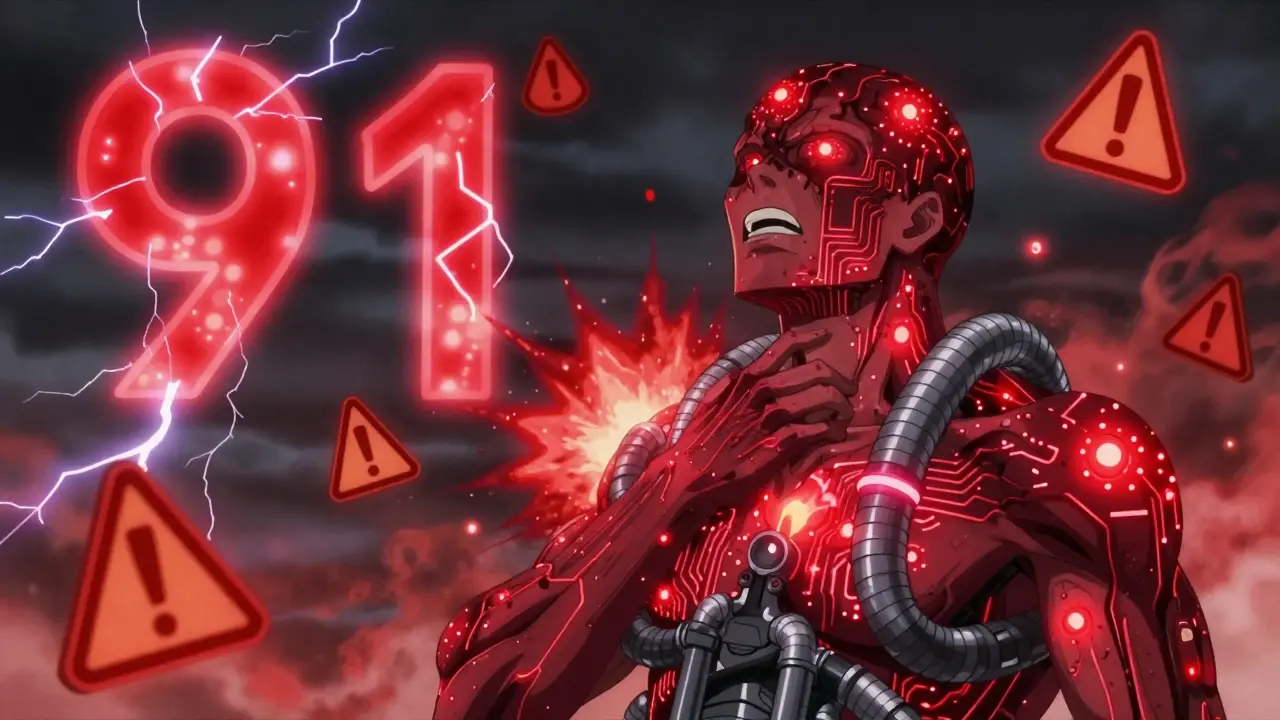
This tool is for informational purposes only. If you are experiencing a medical emergency, call 911 immediately.
You took your pill like always. But five minutes later, your skin broke out in hives. Your throat feels tight. You’re dizzy. Should you call your doctor or 911? This isn’t a guess game. Waiting too long can cost you your life. Knowing the difference between a bothersome side effect and a life-threatening reaction saves lives - and it’s simpler than you think.
Not All Reactions Are the Same
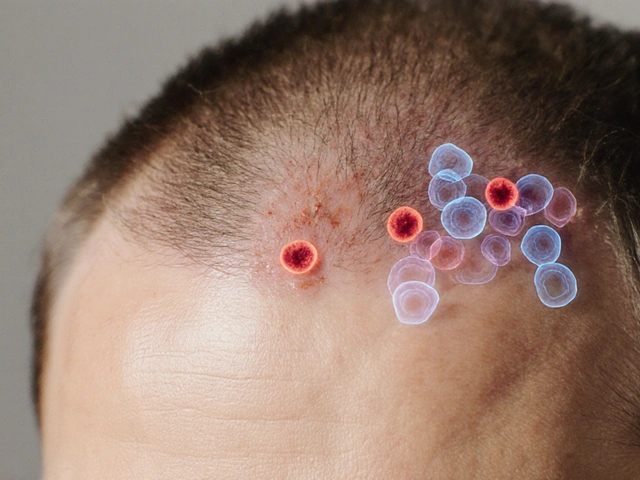
Medications can cause all kinds of reactions. Some are annoying. Others are deadly. A stomachache after taking ibuprofen? That’s a common side effect. A rash that itches but doesn’t spread? Probably not an emergency. But if that same rash shows up with vomiting, swelling, or trouble breathing - now you’re in danger. The key isn’t just the symptom. It’s the combination. One symptom alone? Maybe just a side effect. Two or more systems involved? That’s a red flag. For example, if you have hives and nausea, that’s far more likely to be a true allergy than nausea alone. The American College of Allergy, Asthma, and Immunology says this clearly: when multiple body systems react at once, it’s not just a side effect - it’s an allergic emergency.Call 911 Immediately If You Have These Symptoms
If you experience any of these, don’t wait. Don’t text your doctor. Don’t drive yourself. Call 911 right now:- Swelling of the tongue, lips, or throat
- Wheezing, stridor (that high-pitched, squeaky breathing sound), or trouble catching your breath
- Feeling like your throat is closing
- Weak, fast, or pounding heartbeat
- Dizziness, fainting, or feeling like you’re going to pass out
- Low blood pressure - you might feel cold, clammy, or suddenly very pale
- Vomiting or diarrhea along with skin symptoms like hives or flushing
- Seizure or loss of consciousness
When You Can Wait - But Not Too Long
If your reaction is limited to one thing - like a mild rash, isolated itching, or a slight headache - you probably don’t need 911. But you still need help. Contact your doctor or visit urgent care within 24 hours. Examples of non-emergency reactions:- A flat, red rash that doesn’t spread
- Itching without swelling or breathing issues
- Mild nausea or upset stomach with no other symptoms
- Fatigue or drowsiness that’s new but not extreme
Epinephrine Isn’t Optional - It’s Your Lifeline
If you’ve been prescribed an epinephrine auto-injector (like an EpiPen), use it at the first sign of a severe reaction. Don’t wait for symptoms to get worse. Don’t think, “Maybe it’ll pass.” Epinephrine works fast. It opens your airways. It raises your blood pressure. It stops the reaction in its tracks. The Food Allergy Research & Education organization says: “When in doubt, use it!” And here’s what no one tells you: you still need to call 911 after using epinephrine. One shot might not be enough. Symptoms can come back - sometimes hours later. The Mayo Clinic warns: “You will still need to call 911 or go to the ER after administering epinephrine because one injection may not be enough, and you may have a delayed reaction.” Emergency crews carry more epinephrine. They can monitor your heart, give IV fluids, and watch for rebound reactions. Skipping the ER after using your auto-injector is like putting out a fire with a water bottle and walking away. The embers are still glowing.What About Kids and Elderly?
Children and older adults are at higher risk. Kids often can’t tell you what’s wrong. Older adults may have heart conditions that make reactions more dangerous. But here’s the truth: even if you have heart disease, you should still use epinephrine if you’re having anaphylaxis. The risk of dying from an allergic reaction is far greater than the risk of a temporary spike in heart rate from epinephrine. The National Institute of Allergy and Infectious Diseases says epinephrine is the first-line treatment for a reason - it saves lives. Don’t hold back because you’re scared of side effects. The side effects of anaphylaxis? They’re permanent.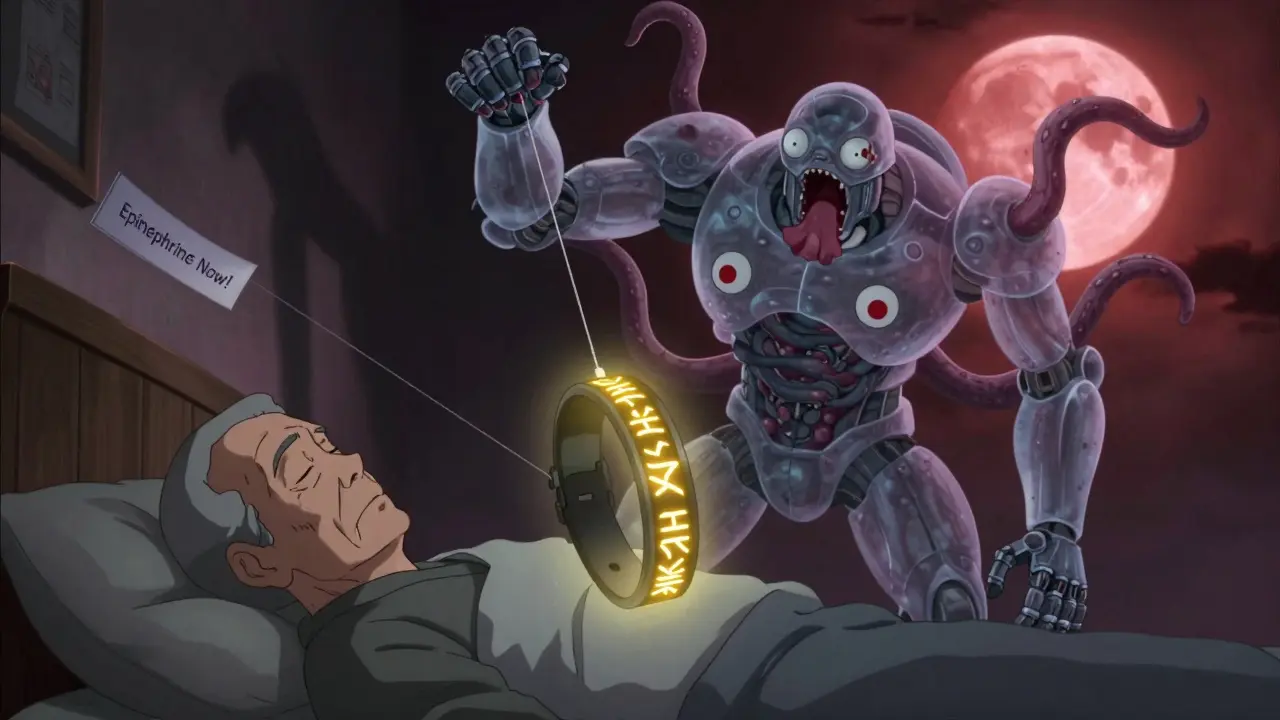



Joie Cregin
January 18, 2026 AT 06:56So I took amoxicillin last year and got this weird little rash-just a few spots, no big deal. Thought it was laundry detergent. Turns out? Two days later I was in the ER with swelling. I didn’t connect the dots until my mom screamed at me to call 911. Don’t be like me. If your skin’s mad at you and your throat feels like it’s trying to close shop? Just. Call. Them.
Epinephrine isn’t scary-it’s your body’s emergency override. Use it like you’re hitting the ‘undo’ button on a glitchy app. Then call 911 anyway. Even if you feel fine. Trust me.
Also, wear a medical bracelet. I didn’t. Now I have one that says ‘ALLERGIC TO PENICILLIN’ in glitter font. Yeah. I’m that person. And I’m proud.
Rob Deneke
January 18, 2026 AT 13:26Just call 911 if you feel weird after a pill no matter what your doctor says. I had a friend who waited two hours to text his GP and ended up on a ventilator. The system fails people every day. Don’t be a statistic. EMTs don’t judge. They show up. That’s all you need.
Epinephrine saves lives. Not your phone. Not your notes. Not your ‘maybe it’ll pass’ thoughts.
Chelsea Harton
January 20, 2026 AT 09:54One symptom maybe chill. Two? Run. Your body doesn’t send invites. It sends warnings. And if you ignore it? It doesn’t yell louder. It just shuts down.
Also epinephrine isn’t magic. It’s a pause button. You still need the ambulance. Always.
Nick Cole
January 20, 2026 AT 16:22People waste time texting doctors like it’s a group chat. You’re having anaphylaxis. Not a bad Yelp review. If your throat is closing, you don’t need a reply from Dr. Patel at 3 AM. You need oxygen, epinephrine, and someone who knows how to intubate. Call 911. Period.
I’ve seen people die because they waited for a ‘second opinion.’ There is no second opinion when your airway is collapsing. Just call. Now.
Riya Katyal
January 21, 2026 AT 12:03Oh wow so if I get a rash after taking Advil I’m supposed to scream into the void and summon the fire department? Maybe next time I’ll just take a nap and hope my throat remembers how to breathe. 🙄
Also why does everyone act like epinephrine is a magic wand? It’s literally adrenaline. You’re just injecting yourself with a panic attack.
waneta rozwan
January 22, 2026 AT 05:19THIS IS WHY AMERICA IS DYING. People think they can ‘wait and see’ when their body is screaming for help. I’ve seen it. A woman in my yoga class took a new antibiotic. Said she had ‘a little itch.’ Three hours later? Cardiac arrest. No EpiPen. No 911. Just… gone.
And now? Her husband posts memes about ‘overreacting.’
Wake up. Your life isn’t a TikTok trend. This isn’t drama. It’s biology. And biology doesn’t care how ‘chill’ you are.
Nicholas Gabriel
January 23, 2026 AT 09:49Let me be very clear, here: if you experience ANY combination of symptoms-such as hives, nausea, dizziness, swelling, difficulty breathing, or a rapid heartbeat-immediately call 911, do not delay, do not hesitate, do not try to drive yourself, do not wait for a response from your doctor, do not assume it’s ‘just a side effect,’ and do not rely on Google. Epinephrine is not optional, it is essential, and you must still go to the ER even after using it, because rebound reactions are real, dangerous, and often fatal if ignored. Please, for the love of everything good, educate yourself, carry your EpiPen, and trust your instincts.
Cheryl Griffith
January 23, 2026 AT 19:50I used to think ‘mild’ reactions weren’t worth worrying about. Then I had a friend who got a rash after a Z-pack. Said it was ‘just a little itchy.’ Three days later, her liver started failing. DRESS syndrome. It’s rare, but it’s real.
Even if it seems small? Call your doctor within 24 hours. Don’t wait. Don’t ‘see how it goes.’ Your body doesn’t give second chances. And if you’re ever in doubt? Call 911. Better to be embarrassed than dead.
Jody Fahrenkrug
January 25, 2026 AT 11:45My grandma took a new blood pressure med and got a rash. She didn’t say anything for a week. Thought it was dry skin. Turns out it was a drug reaction that nearly killed her. Now she wears her EpiPen on a necklace. And she tells everyone who’ll listen.
So yeah. Just call 911. It’s not dramatic. It’s smart.
Kasey Summerer
January 26, 2026 AT 13:49Y’all know what’s wild? We’ll call 911 for a stubbed toe but ignore a throat closing because ‘maybe it’s just stress.’ 🤦♂️
Also, epinephrine is basically your body’s cheat code. Use it. Then call 911. Don’t be that guy who thinks ‘one shot is enough’ and then dies in the parking lot. 😅
Also, wear the bracelet. Even if it says ‘ALLERGIC TO PINEAPPLE’ and you’re not. People remember weird things.
Ryan Hutchison
January 28, 2026 AT 10:52Why are we even having this conversation? In America, you don’t need to Google this stuff. You need to be tough. If you can’t handle a little rash or dizziness, maybe you shouldn’t be taking meds at all. We’ve got people overseas who take penicillin without a hospital nearby. You think they’re calling 911 for a sneeze?
Stop being weak. Epinephrine? That’s for people who can’t handle their own bodies. Just tough it out. That’s how we built this country.
Melodie Lesesne
January 28, 2026 AT 21:15I’m so glad this was posted. My sister had a reaction to a new antidepressant and thought she was just ‘anxious.’ She didn’t realize her tongue was swelling until she couldn’t speak. We called 911 and she’s alive today because of it.
Don’t second-guess your body. It’s smarter than your brain. If something feels wrong after a pill? Act. Fast. And tell your friends. This info saves lives.
Corey Sawchuk
January 29, 2026 AT 14:33My cousin took a new antibiotic. Got a rash. Didn’t say anything. Two days later he was in ICU with multi-organ failure. Turns out it was DRESS. He’s fine now. But he’s got a new rule: if a pill makes you feel weird? Call your doctor. If it makes you feel like you’re dying? Call 911.
And carry your EpiPen. Even if you think you’ll never need it. You never know.