Aminoglycoside Ototoxicity Risk Calculator
Personal Risk Assessment
Calculate your risk of hearing loss or balance damage from aminoglycoside antibiotics based on key factors from the article.
When you’re fighting a life-threatening infection, antibiotics are a lifeline. But for some people, one of the most powerful classes of these drugs-aminoglycosides-can quietly steal their hearing and balance without warning. This isn’t rare. In fact, aminoglycoside ototoxicity affects between 20% and 47% of patients who receive these antibiotics, and for many, the damage is permanent.
What Exactly Is Aminoglycoside Ototoxicity?
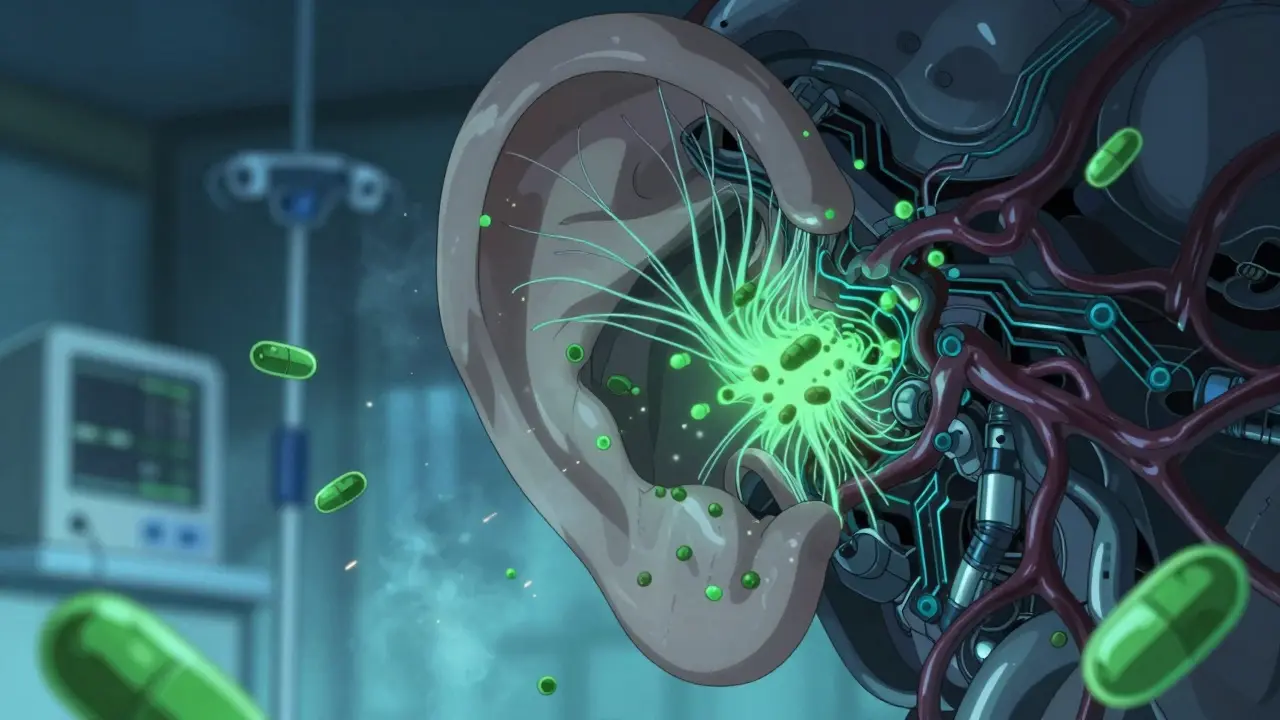
Aminoglycosides are a group of antibiotics that include gentamicin, amikacin, tobramycin, and streptomycin. They’re used when other drugs fail-often for severe infections like sepsis, multidrug-resistant tuberculosis, or complicated urinary tract infections. They work by killing bacteria at the cellular level, but they don’t discriminate. Once in the body, they can slip into the inner ear and start destroying the tiny hair cells that turn sound and movement into signals your brain understands. These hair cells don’t regenerate. Once they’re gone, the hearing loss and balance problems don’t come back. That’s why aminoglycoside ototoxicity is so dangerous: it’s irreversible.How Do These Antibiotics Damage Your Ears?
Aminoglycosides enter the inner ear through the bloodstream, crossing the blood-labyrinth barrier near the stria vascularis. In some cases, they can also get in through the round window membrane, especially if there’s inflammation or an infection nearby. Once inside, they trigger a chain reaction:- They overactivate NMDA receptors, leading to a flood of nitric oxide and free radicals
- These toxins damage mitochondria-the energy factories inside hair cells
- Cells start dying through both apoptosis (programmed death) and necrosis (sudden rupture)
- Autophagy, the cell’s cleanup system, gets hijacked and turns destructive
Why Do Some People Get Hit Harder Than Others?
Not everyone who gets aminoglycosides loses their hearing. But some people are walking time bombs. A genetic mutation in mitochondrial DNA-specifically the A1555G or C1494T variants-makes hair cells far more vulnerable. People with these mutations can suffer severe hearing loss after just one or two doses. The OtoSCOPE® genetic test can detect these mutations with over 94% accuracy. Yet, only a small fraction of hospitals screen for them before treatment. In places where this test isn’t available, doctors are flying blind. Even without genetic risk, other factors stack the deck:- Existing high-frequency hearing loss? You’re 3.2 times more likely to lose more hearing.
- Recent loud noise exposure? Ototoxicity can spike by up to 52%.
- Infection with endotoxins? Inflammation opens the door for 63% more drug to enter the ear.
Hearing Loss vs. Balance Problems
Aminoglycosides don’t just hurt your hearing-they wreck your balance. About 15% to 30% of patients develop vestibular damage, which means dizziness, unsteadiness, blurred vision when moving their head (oscillopsia), and trouble walking in the dark. Unlike cisplatin, which mainly attacks low-frequency hearing, aminoglycosides target both high-frequency hearing and the vestibular system equally. That’s why patients often describe it as losing both their hearing and their sense of direction. Some can’t stand without holding onto a wall. Others feel like they’re on a boat even when standing still.
Who’s Most at Risk?
The highest rates of ototoxicity come from patients treated for multidrug-resistant tuberculosis-68% of reported cases. In low-resource settings, where aminoglycosides are the only affordable option, this is a silent epidemic. The WHO reports that 80% of all aminoglycoside use happens in places with no access to hearing tests or genetic screening. Other high-risk groups:- Newborns in NICUs treated for sepsis
- Patients with kidney disease (since aminoglycosides are cleared by the kidneys)
- People on long courses (more than 7 days)
- Those already taking other ototoxic drugs like loop diuretics
Can You Prevent It?
Yes-but only if you’re being monitored. The American Speech-Language-Hearing Association recommends:- Baseline hearing test within 24 hours of starting treatment
- Follow-up tests every 48 to 72 hours using high-frequency audiometry (9-16 kHz)
- Therapeutic drug monitoring: keeping peak and trough levels within safe ranges
What’s Being Done to Fix This?
There’s real hope on the horizon. In 2023, the FDA gave Fast Track status to ORC-13661, a drug that, when given alongside amikacin, preserved 82% of hair cells in clinical trials. It’s not yet approved, but early results are promising. Researchers at St. Jude are testing compounds that block MET channels-the exact entry point where aminoglycosides invade hair cells. In mice, these blockers prevented hearing loss by 25-30 dB across all frequencies. Gene therapy is also advancing. A project funded by the Oak Foundation showed a 67% reduction in ototoxicity in mice with mitochondrial mutations by repairing the faulty gene. But these solutions won’t help millions in low-income countries unless they become cheap, simple, and widely available.
What Patients Are Saying
On Reddit’s r/audiology, 78% of people who reported aminoglycoside exposure said they lost hearing permanently. 63% still have tinnitus years later. On the Hearing Loss Association forum, 89% said they were never warned about the risk before treatment. One patient wrote: “I was told it was just a strong antibiotic. No one mentioned I might never hear my daughter’s voice clearly again.”What You Should Do
If you or someone you love is being prescribed an aminoglycoside:- Ask: “Is there a safer alternative?”
- Ask: “Can we test my hearing before and during treatment?”
- Ask: “Do you screen for mitochondrial mutations?”
- Ask: “Will you monitor drug levels?”
The Bigger Picture
Aminoglycosides are still used because we have few options against superbugs. But we’re treating the infection without protecting the person. The rise of antibiotic resistance means we’ll keep needing these drugs. That makes prevention not just a medical issue-it’s an ethical one. We have the tools: genetic screening, hearing monitoring, otoprotectants. What’s missing is the will to use them. The next time a doctor says, “This antibiotic is safe,” ask: “Safe for what?”Can aminoglycoside hearing loss be reversed?
No. Once the hair cells in the inner ear die from aminoglycoside exposure, they do not regenerate. The hearing loss and balance problems are permanent. Early detection can stop further damage, but lost function cannot be restored with current treatments.
How long does it take for aminoglycosides to cause hearing loss?
Damage can begin within 24 to 48 hours, but it often takes 5 to 10 days of treatment before it becomes detectable on standard hearing tests. High-frequency audiometry can pick up changes as early as day 3. Some patients report sudden hearing loss after just one or two doses, especially if they have genetic risk factors.
Are there any warning signs before hearing loss happens?
Yes. Early signs include ringing in the ears (tinnitus), muffled hearing, trouble understanding speech in noisy places, or a feeling of fullness in the ears. Balance problems like dizziness, unsteadiness, or blurred vision when moving the head can also appear before hearing loss is obvious. These symptoms should never be ignored.
Can I still get aminoglycosides if I have a family history of hearing loss?
You should be tested for mitochondrial DNA mutations (A1555G or C1494T) before receiving aminoglycosides. If you carry one of these mutations, the risk of severe, rapid hearing loss is extremely high. In many cases, doctors will avoid aminoglycosides entirely and choose safer alternatives. Genetic screening is the best way to prevent disaster.
Is it safe to use aminoglycosides in children or newborns?
They are used in newborns for life-threatening infections like sepsis, but the risk of ototoxicity is higher due to immature kidney function and developing inner ears. Whenever possible, alternatives are preferred. If aminoglycosides are necessary, strict monitoring with daily high-frequency audiometry and blood level checks is essential. Many NICUs still lack these protocols, putting infants at unnecessary risk.
Can noise exposure make aminoglycoside damage worse?
Yes. Even moderate noise exposure before or during treatment can double or triple the damage. Loud environments-like construction sites, concerts, or busy hospitals-can turn a safe dose into a dangerous one. Patients should avoid loud noise during and for at least 2 weeks after treatment.
What should I do if I think I’ve developed ototoxicity?
Stop the medication immediately (only under medical supervision) and get a full hearing and vestibular evaluation from an audiologist. Don’t wait. Early intervention can prevent further damage, even if lost hearing can’t be restored. Report your symptoms to your doctor and ask for a referral to an ototoxicity specialist.
Are there any new drugs or treatments that protect hearing during aminoglycoside therapy?
Yes. ORC-13661, an experimental otoprotectant, showed 82% hair cell preservation in Phase II trials when given with amikacin. Other compounds targeting MET channels in hair cells have shown success in animal studies. While none are widely available yet, clinical trials are ongoing. Ask your doctor if you qualify for a trial.


Rob Webber
January 30, 2026 AT 01:17My cousin got gentamicin for a UTI. Now she can't hear her own kids. No warning. No test. Just 'it's rare.' It's not rare. It's negligence.
calanha nevin
January 31, 2026 AT 03:22Healthcare systems prioritize cost over consequence. We screen for every minor risk except the ones that permanently alter someone's life. We need mandatory pre-treatment hearing baselines for all high-risk patients. Not optional. Not 'if available.' Mandatory.
Claire Wiltshire
January 31, 2026 AT 17:32We have the science. We have the tools. What we lack is systemic will. I've seen patients lose their hearing after one dose because they had the mutation and no one tested. That's not bad luck. That's a system failure.
If you're prescribed an aminoglycoside, insist on the baseline test. If they say no, ask for a second opinion. Your ears are irreplaceable.
Darren Gormley
February 2, 2026 AT 15:25Also, ORC-13661? That's just another pharma fairy tale. 82% preservation in trials? Cool. Now show me the Phase III results. And the price tag. And the insurance coverage. And the 5-year follow-up. Yeah. Thought so.
Sidhanth SY
February 3, 2026 AT 07:59It's heartbreaking. But the real issue isn't just medicine-it's access. We need cheap, portable audiometry devices and low-cost genetic screening kits. Not just for the U.S. and Europe. For everyone.
Beth Cooper
February 3, 2026 AT 11:01Also, the 'fast track' drug? That's just a placebo with a patent. They'll sell it for $50,000 a dose. Meanwhile, the WHO says 80% of use is in low-income countries. So who's really being protected? Not you.
Donna Fleetwood
February 4, 2026 AT 08:34It’s not fair. But it’s not the end. There’s community. There’s hope. And there’s science moving faster than you think.
Bobbi Van Riet
February 4, 2026 AT 08:48But I know. I know it’s the antibiotics. I’ve been researching for weeks. I wish I’d known sooner. I wish someone had told us. Now I’m scared for myself. I’m on antibiotics right now for a sinus infection. Should I refuse them? What do I even ask my doctor? I feel so helpless.
Carolyn Whitehead
February 6, 2026 AT 02:42Now I’m 34. Still have it. Still get dizzy sometimes. I’m not angry. Just… sad. Like I lost something I never knew I had.
Natasha Plebani
February 6, 2026 AT 10:48What we’re witnessing isn’t just toxicity-it’s a failure of systems biology integration in clinical practice. The reductionist model of ‘drug → target’ ignores emergent systemic collapse. Until we treat the ear as an integrated organ-not a bag of cells-we’ll keep repeating this tragedy.
Kelly Weinhold
February 8, 2026 AT 03:50But I still cry when I hear birds. I miss that sound. I miss the quiet moments. Don’t let this happen to you. Ask the questions. Push back. Your hearing is worth it.
Kimberly Reker
February 9, 2026 AT 00:23Most hospitals don’t do this. And that’s the real scandal. Not the drug. The lack of care. We can do better. We just have to choose to.
Eliana Botelho
February 10, 2026 AT 13:06And why are we still using 1950s drugs in 2024? Someone’s making money off this. Probably the same people who sold us cigarettes. It’s not the drug-it’s the entire medical-industrial complex. We’re all just pawns.
Niamh Trihy
February 11, 2026 AT 13:34Please, if you’re a clinician: screen. Monitor. Educate. If you’re a patient: ask. Push. Demand. We owe it to each other to do better.
Diana Dougan
February 12, 2026 AT 18:43Also, 'genetic screening'? That’s gonna be $2,000 and take 3 weeks. By then, the patient’s dead. So thanks for the feel-good article. Real helpful.