When you’re diagnosed with an autoimmune disease like rheumatoid arthritis, multiple sclerosis, or lupus, the next question isn’t just what treatment to take-it’s which treatment fits your life. One pill a day? Daily injections? Monthly infusions? Each option comes with trade-offs: better symptom control versus higher risk of infection, fewer flares versus the chance of a rare but serious side effect. This is where shared decision-making (SDM) isn’t just nice to have-it’s essential.
What Shared Decision-Making Really Means
Shared decision-making isn’t just the doctor giving you a list of options and saying, "What do you want?" It’s a structured conversation where both you and your provider work together to pick the best path forward. You bring your values, lifestyle, fears, and goals. Your provider brings the science-what the data says about how well each treatment works and what risks come with it. This approach became standard care for chronic conditions like autoimmune diseases because traditional models failed. In the old system, doctors decided. In the newer "informative" model, doctors list options and leave you alone to choose. But neither works well when the stakes are high. A 2017 study of over 3,200 people with autoimmune conditions found that those who took part in true shared decision-making were 82% likely to stick with their treatment. Those who didn’t? Only 63%. Why the big difference? Because when you understand the real numbers-and feel heard-you’re more likely to follow through. If you’re a nurse working night shifts, a daily injection might be impossible. If you’re planning a pregnancy, some biologics are off the table. If you’re terrified of needles, an oral drug might be the only option that keeps you compliant. SDM makes space for those realities.The Tools That Make It Work
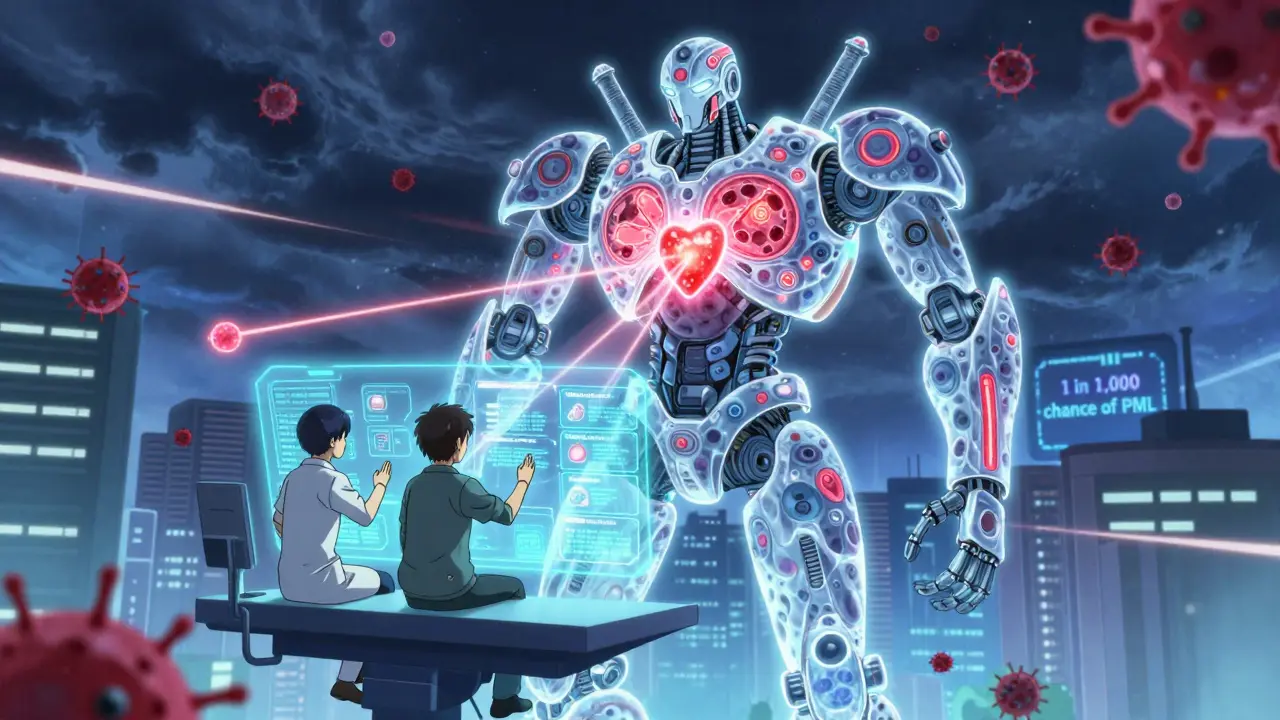
Good shared decision-making doesn’t happen by accident. It needs tools. One of the most common is a decision aid. These aren’t just brochures. They’re evidence-based tools-sometimes videos, apps, or printed booklets-that break down treatment choices with clear numbers. For example, a decision aid for rheumatoid arthritis might say: "With adalimumab, 60 out of 100 people see at least a 20% improvement in symptoms. With methotrexate alone, it’s 50 out of 100. But with adalimumab, you have a 1.8% chance per year of a serious infection. With methotrexate, it’s 1.2%." That’s not vague. That’s concrete. And it’s exactly what patients say they need. The Ottawa Hospital Research Institute developed decision aids for biologics in RA, psoriatic arthritis, and lupus. The Arthritis Foundation has free versions too. These tools use absolute risk-not relative percentages-because "50% lower risk" sounds better than it is. If the baseline risk is 1 in 1,000, cutting it in half still means 1 in 2,000. People need to see the real numbers to make sense of it. For multiple sclerosis, the University of Michigan’s "MS Decisions" tool shows PML risk as "1 in 1,000 over two years" instead of "0.1%"-and patients rate it 4.6 out of 5. Why? Because it matches how people think. We don’t process decimals well. We understand "one in a thousand."How the Conversation Actually Goes
A real shared decision-making visit doesn’t take an hour. It takes about 9 to 14 minutes-broken into three parts.- Team Talk (1-2 minutes): "I want to make sure we’re on the same page. What matters most to you about your treatment?"
- Option Talk (5-7 minutes): "Here are your options. Here’s what the data says about how well each works, and what side effects you might face. Let me show you the numbers."
- Decision Talk (3-5 minutes): "Which option feels right for you? What concerns do you still have?"

When Shared Decision-Making Falls Short
It’s not perfect. And patients know it. A 2020 survey by the National MS Society found that 63% of patients felt rushed during treatment discussions. One woman said, "My neurologist listed three MS drugs in 90 seconds with no discussion of how they’d fit my nursing schedule." That’s not shared decision-making. That’s information dumping. Another problem? Health literacy. A 2022 study in the Journal of Autoimmunity found that patients over 65 and those with lower health literacy got 37% less benefit from digital decision aids-unless they had someone to walk them through it. That’s why clinics that pair digital tools with a nurse or patient navigator see much better results. And then there’s the issue of timing. During a severe flare-when a patient’s joints are swollen, or their vision is blurring-there’s no time for a 10-minute discussion. A 2020 study showed 47% of rheumatologists say SDM is impractical during acute flares. That’s okay. SDM isn’t meant for emergencies. It’s meant for planning the long road ahead.Why It Matters More in Autoimmune Diseases
Autoimmune treatments are uniquely tricky. They don’t just treat symptoms-they change how your immune system works. That means they can help you walk again… or leave you vulnerable to infections that could kill you. Take natalizumab for MS. It cuts relapses by up to 70%. But it carries a risk of PML-a rare brain infection. The FDA says it happens in about 1 out of every 1,000 patients treated. That’s low. But if you’re that one person, it’s everything. Or consider TNF inhibitors for rheumatoid arthritis. They’re great for stopping joint damage. But they raise your risk of tuberculosis, fungal infections, and even certain cancers. The difference between a 1.2% and 1.8% annual risk might seem small. But if you’re a parent with young kids, or you work in a hospital, that extra 0.6% matters. This is where shared decision-making shines. It doesn’t just say, "This drug works." It says, "Here’s what this drug might cost you-and what it might give you. What’s worth it to you?"
What’s Changing Now
The field is evolving fast. In March 2023, the FDA cleared the first AI-powered decision support tool for rheumatoid arthritis: ArthritisIQ. It pulls data from your electronic health record and your own symptom reports to generate a personalized risk-benefit profile. The Multiple Sclerosis Association of America launched the "MS Values Compass" in February 2023-it helps patients rank what matters most: "Can I travel?" "Can I get pregnant?" "Can I keep working?" Insurance companies are catching on too. Medicare Advantage plans now tie 9% of payments to patient experience scores-and shared decision-making is a big part of that. The Choosing Wisely campaign has 17 autoimmune-specific recommendations urging doctors to involve patients in treatment choices. In Europe, the European League Against Rheumatism now requires SDM documentation when starting biologic therapy. As a result, European doctors prescribe biologics more appropriately than U.S. doctors-22% more so, according to a 2022 study.What You Can Do
If you have an autoimmune disease, here’s how to make sure you’re part of the decision:- Ask: "What are my options?" Don’t settle for "We can try this drug."
- Ask: "What does the data say about how well each works?" Ask for percentages, not just "it’s effective."
- Ask: "What are the real risks?" Not "there’s a small chance," but "how many people out of 100 have this side effect?"
- Ask: "Which option fits my life?" If you travel often, work nights, or care for kids, say so.
- Use free tools. The Arthritis Foundation and National MS Society have downloadable decision aids. Print them. Bring them to your appointment.
Final Thought: It’s Not About Being Right. It’s About Being Right for You.
There’s no single best treatment for autoimmune diseases. What works for one person might be dangerous or impractical for another. Shared decision-making doesn’t promise perfection. But it does promise alignment. It brings science and soul together. It turns treatment from something done to you into something chosen with you. And in a world where chronic illness lasts decades, that matters more than ever.What is shared decision-making in autoimmune care?
Shared decision-making is a process where you and your healthcare provider work together to choose a treatment based on both medical evidence and your personal values, lifestyle, and goals. It’s not about the doctor deciding for you, or just giving you a list and walking away. It’s a conversation that includes clear data on risks and benefits, and a focus on what matters most to you.
Why is shared decision-making important for autoimmune diseases?
Autoimmune treatments often have serious trade-offs-like improved symptom control versus higher infection risk. Because these treatments are long-term and affect your daily life, choosing the right one depends on your personal priorities. Shared decision-making ensures your values are part of the equation, which leads to better adherence, fewer side effects, and higher satisfaction.
What tools are used in shared decision-making?
Common tools include decision aids like printed booklets, videos, and digital apps that show exact treatment outcomes and risks. For example, the Arthritis Foundation offers free tools for RA, lupus, and psoriatic arthritis. The MS Values Compass helps patients rank what matters most-like travel, pregnancy, or work. These tools use absolute risk numbers (e.g., "1 in 1,000 chance") instead of vague terms to help you understand real likelihoods.
Can shared decision-making be used during a disease flare?
Usually not. During a severe flare-like sudden joint swelling or vision loss-treatment needs to be fast. Shared decision-making works best for planning long-term treatment, not emergency care. Most providers say it’s impractical during acute flares, but they use it to plan next steps once the flare is under control.
How can I prepare for a shared decision-making appointment?
Before your visit, think about what matters most: your job, family responsibilities, fear of needles, travel plans, or desire to get pregnant. Use free decision aids from the Arthritis Foundation or National MS Society. Write down your questions: "What are the risks?" "How many people have this side effect?" "Which option fits my life?" Bring those notes to your appointment.
Do insurance plans support shared decision-making?
Yes. Medicare Advantage plans now tie 9% of payments to patient experience scores, and shared decision-making is a key part of that. The Choosing Wisely campaign has 17 autoimmune-specific recommendations promoting patient involvement. In Europe, guidelines now require SDM documentation for biologic therapy, improving treatment appropriateness.



Dee Humprey
January 3, 2026 AT 11:32I wish my rheumatologist had used a decision aid when I started on biologics. I had no idea the infection risk was 1.8% per year until I read it on the Arthritis Foundation site myself. Took me three months to even ask the right questions. Don't wait. Print the damn thing and bring it.
Also, if you're on night shifts like me? Say it upfront. No one's gonna guess you're too tired for injections.
Allen Ye
January 3, 2026 AT 19:15What's fascinating here is how this model implicitly rejects the Cartesian dichotomy between patient and provider as separate epistemic agents. Shared decision-making, when done right, dissolves the hierarchy-replacing it with a co-constructed epistemic space where lived experience and clinical evidence are not competing truths but interdependent modalities of knowing. The 82% adherence rate isn't just a statistic-it's a phenomenological validation. We're not talking about compliance anymore. We're talking about ontological alignment. The body doesn't obey commands. It consents. And consent requires dialogue, not directives. This is why the European guidelines mandating SDM documentation are revolutionary-they're not bureaucratic-they're hermeneutic. We're finally treating chronic illness as a narrative, not a protocol.
Clint Moser
January 5, 2026 AT 08:50Did you know the FDA approved ArthritisIQ because Big Pharma funded the trial? Same people who pushed biologics as 'miracle drugs' now say 'shared decision-making'-total smoke and mirrors. They want you to think you're choosing, but the options are all their products. The real risk isn't PML-it's being manipulated into paying $20k/year for a drug that only works for 60% of people. They don't want you to know about methotrexate or sulfasalazine. They want you scared of needles so you'll take the pill that costs 10x more. Wake up.
Also, 'absolute risk' is just a PR trick. 1 in 1000 sounds safe until you're the one who gets PML. Then it's 100%.
Ashley Viñas
January 5, 2026 AT 23:05Oh honey. You brought a printed decision aid to your appointment? How adorable. Did you also wear a 'I ♥ My Immune System' t-shirt? Look, if you can't even interpret a 1.8% risk without a pamphlet, maybe you shouldn't be making medical decisions at all. This isn't IKEA assembly. You need a doctor who knows what they're doing-not someone who's just reading off a script because you printed a PDF from the Arthritis Foundation. I mean, really. The fact that we've lowered the bar this low is embarrassing. If you can't handle a 5-minute conversation with a specialist, maybe you're not ready for biologics. Just sayin'.
Also, 'MS Values Compass'? That sounds like a BuzzFeed quiz.
Jason Stafford
January 7, 2026 AT 09:58They're lying. All of it. The '1 in 1,000' PML risk? That's a lie. The real number is hidden in the FDA's 2019 whistleblower report. The trials were rigged. The side effects were downplayed. And now they're pushing 'decision aids' so you'll feel guilty for not choosing the expensive drug. They don't care if you live. They care if you sign the consent form. They're turning medicine into a sales pitch. And you? You're the product.
They don't want you to know that 70% of biologics are prescribed to people who don't even meet the diagnostic criteria. It's a money machine. And now they've invented 'shared decision-making' to make you feel like you're part of it. You're not. You're the mark.
PS: They know you're reading this. They're tracking you.
Justin Lowans
January 8, 2026 AT 21:24This is one of the most thoughtful, clinically grounded pieces I've read on patient-centered care in years. The emphasis on absolute risk over relative percentages alone deserves a standing ovation. Too many providers default to vague language-'low risk,' 'possible side effect'-which is not just unhelpful, it's unethical. The fact that clinics using pre-visit digital surveys cut consultation time by 3 minutes and improved outcomes? That’s not just efficiency-that’s dignity. And kudos to the European guidelines mandating documentation. We need that here. Medicine shouldn’t be a lottery. It should be a partnership. Thank you for articulating this so clearly.
Vicki Yuan
January 9, 2026 AT 18:35My husband has lupus and we used the Arthritis Foundation’s tool before his last appointment. We printed it, highlighted the risks, and wrote down our top three concerns: travel, fertility, and fatigue. The rheumatologist was shocked-and then thrilled. He said he’d never seen a patient come in so prepared. We got a treatment plan that actually fits our life. No more 'just take this' nonsense. I wish everyone knew this was possible. It’s not about being difficult-it’s about being smart. Bring the paper. Ask the numbers. Say what matters. You deserve that.
Jay Tejada
January 11, 2026 AT 10:28Man, in India we don't even get to choose the first pill, let alone the fancy biologics. My cousin got diagnosed with RA last year. Doctor gave him one medicine, said 'take it, come back in a month.' No talk. No numbers. No decision. Just pay and go. So yeah, I'm glad y'all have these tools. But don't act like this is normal everywhere. We're lucky if we get a doctor who speaks English.
Also, 'MS Values Compass'? Sounds like a dating app for people with autoimmune stuff.
josh plum
January 12, 2026 AT 23:00Everyone here is acting like this is some revolutionary breakthrough. Newsflash: doctors have been doing this for decades. The only difference now is they're being forced to document it because of insurance. And the tools? They're just marketing. The real reason adherence went up? Because patients got scared of losing their insurance if they didn't comply. You think people are choosing treatments because they 'feel heard'? Nah. They're choosing because they're scared of being labeled 'noncompliant' and getting cut off. This isn't empowerment. It's surveillance with a smile.
John Ross
January 14, 2026 AT 14:05Let’s not romanticize this. SDM is a structural band-aid for a broken system. We’re talking about a 14-minute window in a 10-minute visit. The tools are great, but they’re designed for patients who already have health literacy, internet access, and time to print PDFs. What about the single mom working two jobs? The undocumented immigrant? The person without a smartphone? SDM, as it’s currently implemented, is a privilege. It’s not equity. It’s a checklist for the already-advantaged. The real innovation would be funding patient navigators in every clinic-not just fancy apps. But that costs money. And money talks louder than empathy.
Brendan F. Cochran
January 16, 2026 AT 02:34Y’all are overthinking this. Just take the damn pill. If you're scared of needles, take the pill. If you want to get pregnant, ask your doc. If you're tired, rest. Stop reading all these PDFs and start living. I've had RA for 12 years. I didn't need no 'compass' or 'aid'. I just did what the doctor said. And I'm still walking. You think you're being empowered? You're just wasting time. Go outside. Walk. Eat real food. Stop obsessing over 0.6% risk. It's not gonna kill you. Your anxiety is.