Medication Interaction Risk Checker
Check Your Medication Interactions
Enter your medications to see if any dangerous combinations could cause a hypertensive crisis. This tool is based on the medical information in the article above.
How to Use This Tool
WARNING: This tool is for informational purposes only and does not replace medical advice. If you experience symptoms of a hypertensive crisis (severe headache, chest pain, blurred vision, confusion), call 911 immediately.
Always tell your doctor and pharmacist about all medications you take—including over-the-counter drugs, supplements, and herbal products.
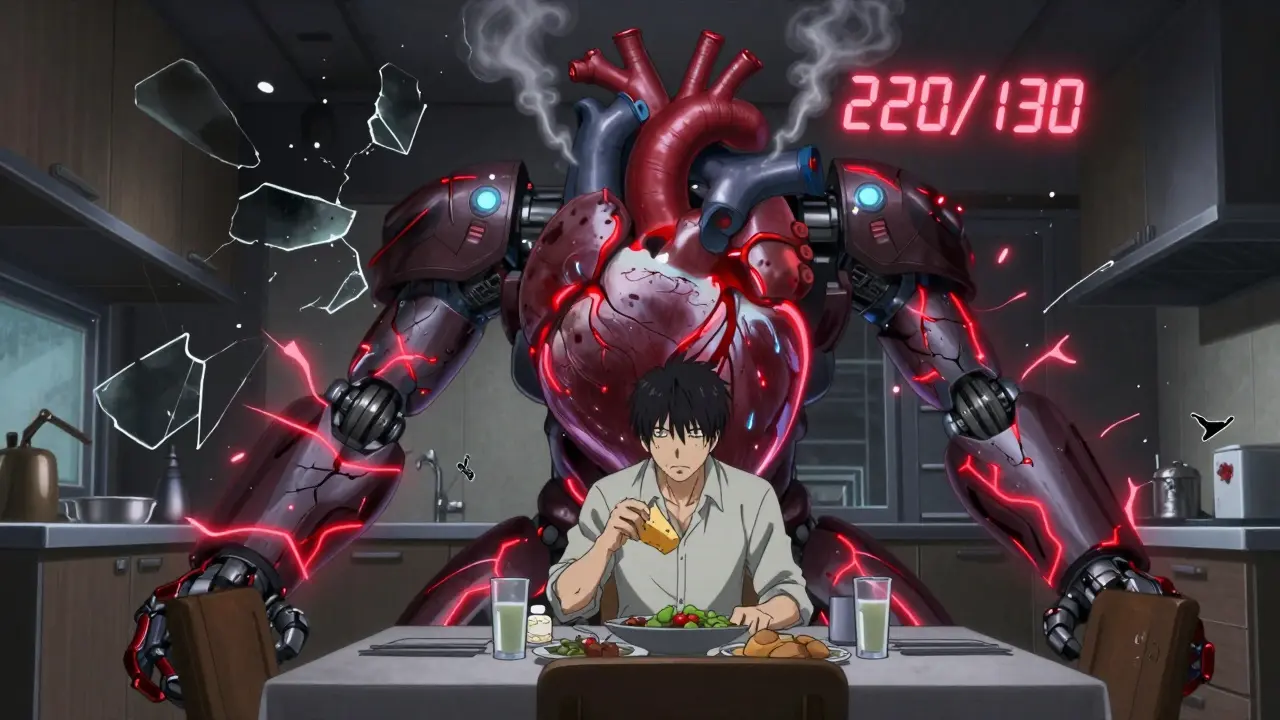
When your blood pressure spikes to 220/130 in minutes-while you’re just eating cheese and taking your antidepressant-you don’t just feel dizzy. You feel like your head might explode. This isn’t a horror movie. It’s a real, preventable medical emergency called a hypertensive crisis, and it’s often triggered by something as simple as mixing two common medications-or even a snack you didn’t think twice about.
What Exactly Is a Hypertensive Crisis?
A hypertensive crisis happens when your blood pressure shoots past 180/120 mmHg, and your body can’t handle the pressure. It’s not just high blood pressure. It’s high blood pressure that’s actively damaging your brain, kidneys, heart, or eyes. The difference between a dangerous spike and routine hypertension? Damage. If your blood pressure stays this high for even an hour, tiny blood vessels start leaking, organs swell, and strokes or kidney failure can follow.
Doctors split these crises into two types: urgency and emergency. Urgency means your pressure is sky-high but your organs are still okay. Emergency means your organs are already under attack. The emergency type is the one that lands you in the ICU. And guess what? About one in five of these emergencies aren’t caused by untreated high blood pressure at all. They’re caused by drugs-either alone or, more dangerously, when they mix.
Drugs That Can Trigger a Blood Pressure Bomb
Not all medications are created equal when it comes to blood pressure. Some are fine on their own. Others? They turn into time bombs when paired with something else.
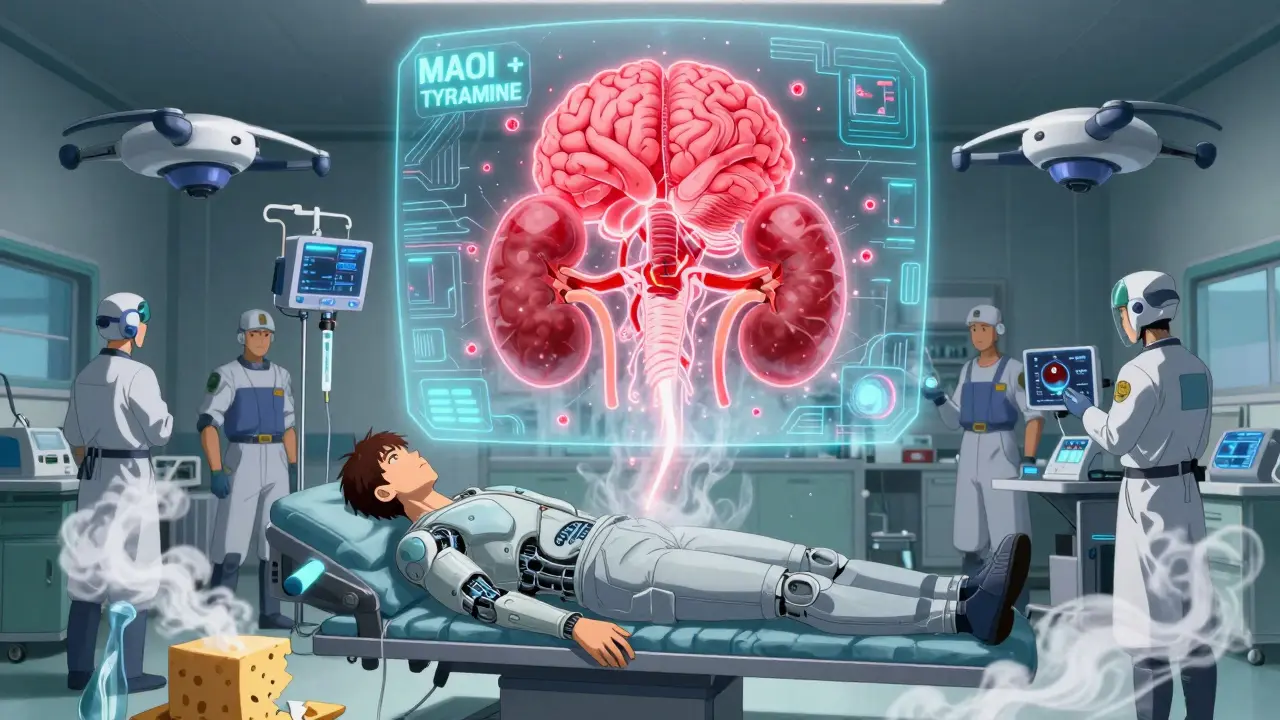
Take MAOIs-medications like phenelzine or selegiline, often prescribed for depression or Parkinson’s. They work by blocking an enzyme that breaks down norepinephrine. That’s good for mood. But if you eat aged cheese, cured meats, or even tap beer while on them, tyramine (a natural compound in those foods) floods your system. Your body can’t break it down, so it pushes out massive amounts of norepinephrine. Blood pressure spikes-sometimes over 250 mmHg-in under an hour. One patient in a 2023 Reddit thread described waking up with 220/130 after eating cheddar cheese with his selegiline. He spent three days in the ICU. He still won’t touch cheese.
Then there’s venlafaxine. This common antidepressant is fine for most people under 225 mg/day. But above that dose, it starts acting like a stimulant. Studies show diastolic pressure climbs above 90 mmHg in up to 40% of users on high doses. Mix it with an over-the-counter decongestant like pseudoephedrine-or worse, Adderall-and you’re playing Russian roulette with your brain. A 2021 study found venlafaxine-amphetamine combinations caused 40% more hypertensive emergencies than historical data predicted.
Cocaine is another silent killer. Alone, it spikes blood pressure. But when someone on a beta-blocker like propranolol uses it? The beta-blocker blocks the heart’s response, but leaves the blood vessels wide open to unopposed adrenaline. Result? Systolic pressure hits 220 mmHg or higher within 30 minutes. This combo has killed people in their 30s who thought they were just being careful with their meds.
And don’t forget licorice. Yes, candy. Black licorice contains glycyrrhizin, which blocks an enzyme that normally keeps cortisol from acting like a mineralocorticoid. That means your body starts retaining salt and water like a sponge. Blood volume goes up. Potassium drops. Blood pressure climbs-sometimes slowly over weeks, but it doesn’t stop until you quit the candy. One patient in a 2022 case report had his BP normalize in 14 days after stopping his daily licorice habit. He didn’t even know it was the problem.
Why Do Doctors Miss This So Often?
Here’s the scary part: in 65% of hypertensive crisis cases, doctors don’t even check the patient’s meds. A 2019 European Society of Hypertension study found only 35% of ER physicians routinely ask about drug interactions when someone shows up with extreme hypertension. They assume it’s just bad hypertension. They don’t ask about supplements. They don’t ask about over-the-counter cold meds. They don’t ask about that bag of licorice the patient’s been eating for years.
Patients aren’t helping either. A 2021 survey found 68% of people who had a drug-induced crisis had complained of unexplained headaches or blurry vision before-but their doctors never connected the dots. Why? Because no one told them to. And most patients don’t know to mention that they take St. John’s Wort with their antidepressant, or that they use Sudafed for their sinus infection while on cyclosporine after a kidney transplant.
Cyclosporine, used in transplant patients, causes high blood pressure in up to half of users. But when doctors see rising pressure, they often think it’s organ rejection. So they increase the immunosuppressant dose. That makes the hypertension worse. It’s a vicious loop. A 2019 study found 55% of these cases were misdiagnosed because no one asked about the meds.
What Should You Do If You’re on High-Risk Medications?
If you’re taking any of these, you need a plan:
- MAOIs: Avoid aged cheese, cured meats, soy sauce, tap beer, and red wine. Use the MAOI Diet Helper app-it cut non-compliance by 78% in a Mayo Clinic trial. Wait at least 4 weeks after stopping an irreversible MAOI before starting any new antidepressant.
- Venlafaxine: If you’re on more than 225 mg/day, get your blood pressure checked every month. Tell your doctor if you get headaches, nosebleeds, or vision changes. Don’t take decongestants without checking first.
- Cyclosporine: Monitor your BP weekly for the first 3 months. If it rises, don’t assume rejection-ask for a medication review.
- Any stimulant or weight-loss drug: Avoid if you have any history of high blood pressure. Phentermine combined with SSRIs is a known danger zone.
- Over-the-counter meds: Read labels. Pseudoephedrine, phenylephrine, and even some cough syrups can trigger crises. If you’re on any prescription for depression, anxiety, or heart issues, assume OTC meds are risky until proven safe.
Keep a list of every medication, supplement, and herbal product you take. Bring it to every appointment-even if you think it’s harmless. That ginseng tea? That fish oil? That turmeric pill? They all interact.
What Happens in the ER?
If you end up in the emergency room with a hypertensive crisis, time is everything. Doctors don’t just lower your pressure slowly. They need to stop the damage now.
For MAOI-tyramine crises? The gold standard is IV phentolamine. It works in under 20 minutes and has a 92% success rate. For cyclosporine-induced cases? Calcium channel blockers like amlodipine work best. For cocaine or stimulant-related spikes? Labetalol is the go-to-it blocks both adrenaline and heart rate.
But here’s the catch: none of these drugs work if the cause isn’t identified. If the ER team doesn’t know you took selegiline and ate blue cheese, they’ll treat the symptom, not the cause. And if you’re on MAOIs, giving certain other drugs-like meperidine or dextromethorphan-can trigger serotonin syndrome on top of the crisis. That’s a double emergency.

The Bigger Picture: Why This Is Getting Worse
This isn’t just about a few bad combos. It’s about a broken system.
Antidepressant prescriptions are rising 13% a year. Weight-loss drugs like phentermine and semaglutide are now widely available. People are on more meds than ever. The average 65-year-old takes five prescriptions. That’s a recipe for disaster.
Drug labels? Only 12% of decongestants warn about hypertension risk. Even after the FDA mandated black box warnings on MAOIs in 2022, many OTC products still don’t say a word. And 78% of high-risk medications have labels that don’t clearly warn about off-label dangers.
Meanwhile, AI tools are being developed to prevent this. The NIH’s new Hypertension Interaction Alert System can predict severe reactions with 92% accuracy by analyzing 15,000+ drug interactions. It’s in phase 3 trials. But until it’s in every EHR, you’re your own best defense.
What You Can Do Today
You don’t need to be a doctor to save your life.
- Write down every pill, patch, and potion you take-even the ones you think are "natural."
- Ask your pharmacist: "Could any of these raise my blood pressure if I mix them?"
- If you’re on an MAOI, delete your cheese and soy sauce from your grocery list-until you talk to your doctor.
- Get a home BP monitor. Check it weekly if you’re on venlafaxine, cyclosporine, or any stimulant.
- If you feel a pounding headache, chest tightness, or blurred vision after starting a new med or eating something new-call 911. Don’t wait. Don’t take an aspirin and hope it goes away.
Severe hypertensive crisis isn’t rare. It’s silent. It’s avoidable. And it’s happening to people who thought they were doing everything right. Your meds aren’t the enemy. But if you don’t know how they play together, you’re playing with fire.
Can over-the-counter cold medicines cause a hypertensive crisis?
Yes. Decongestants like pseudoephedrine and phenylephrine are common triggers. They constrict blood vessels to reduce nasal swelling, but that same effect spikes blood pressure. People on MAOIs, venlafaxine, or cyclosporine are at highest risk. Even if you’re not on those meds, if you have high blood pressure, these OTC drugs can push you into crisis. Always check with your pharmacist before taking them.
Is licorice really dangerous for blood pressure?
Yes-especially black licorice. It contains glycyrrhizin, which tricks your body into acting like it has too much aldosterone. This causes salt retention, low potassium, and high blood pressure. Just 2 ounces a day for two weeks can trigger a crisis in sensitive people. Red licorice usually doesn’t contain it, but always check the label. Stopping licorice can normalize BP in 10-14 days.
How long should I wait between stopping an MAOI and starting a new antidepressant?
For reversible MAOIs like moclobemide, 24 hours is usually enough. For irreversible ones like phenelzine or tranylcypromine, wait 4 to 5 weeks. For selegiline patches, wait at least 14 days. Going too soon can cause serotonin syndrome or a hypertensive crisis. Never switch without your doctor’s guidance.
Can I still drink alcohol if I’m on blood pressure meds?
It depends. Moderate alcohol (one drink a day) is usually fine for most people. But if you’re on MAOIs, avoid alcohol completely-it can trigger a dangerous spike. Also, alcohol can make drugs like venlafaxine or cyclosporine harder on your liver and blood pressure. If you’re unsure, skip it. It’s not worth the risk.
What should I do if I think I’m having a hypertensive crisis?
Call 911 or go to the ER immediately. Don’t wait. Don’t try to lower it yourself with home remedies. Symptoms include severe headache, chest pain, blurred vision, nausea, confusion, or shortness of breath. While waiting for help, sit quietly, avoid caffeine, and don’t take extra blood pressure pills unless instructed. Speed matters-every minute counts.


Dolores Rider
January 23, 2026 AT 17:48Jenna Allison
January 25, 2026 AT 02:48Sharon Biggins
January 26, 2026 AT 12:27John McGuirk
January 27, 2026 AT 19:21Michael Camilleri
January 29, 2026 AT 00:04lorraine england
January 30, 2026 AT 19:39Darren Links
January 31, 2026 AT 13:44Kevin Waters
January 31, 2026 AT 18:05Jamie Hooper
February 1, 2026 AT 22:26Husain Atther
February 3, 2026 AT 16:29