Why Heat Turns Ordinary Medications Into Hidden Dangers for Seniors
It’s not just the heat that’s dangerous for seniors-it’s what happens when that heat meets their daily pills. Many common medications quietly mess with the body’s ability to cool down, hold onto water, or sense when it’s dehydrated. On a 95°F day, a senior taking just one of these drugs might not feel thirsty, sweat less, or lose too much salt without even knowing it. By the time they feel dizzy or confused, it’s often too late. The CDC says more than 600 Americans die every year from heat-related causes, and seniors on certain medications are at the highest risk. This isn’t rare. Nearly 87% of adults over 65 take two or more prescription drugs. That means most seniors are already walking a tightrope when summer hits.
Medications That Turn Up the Heat Risk
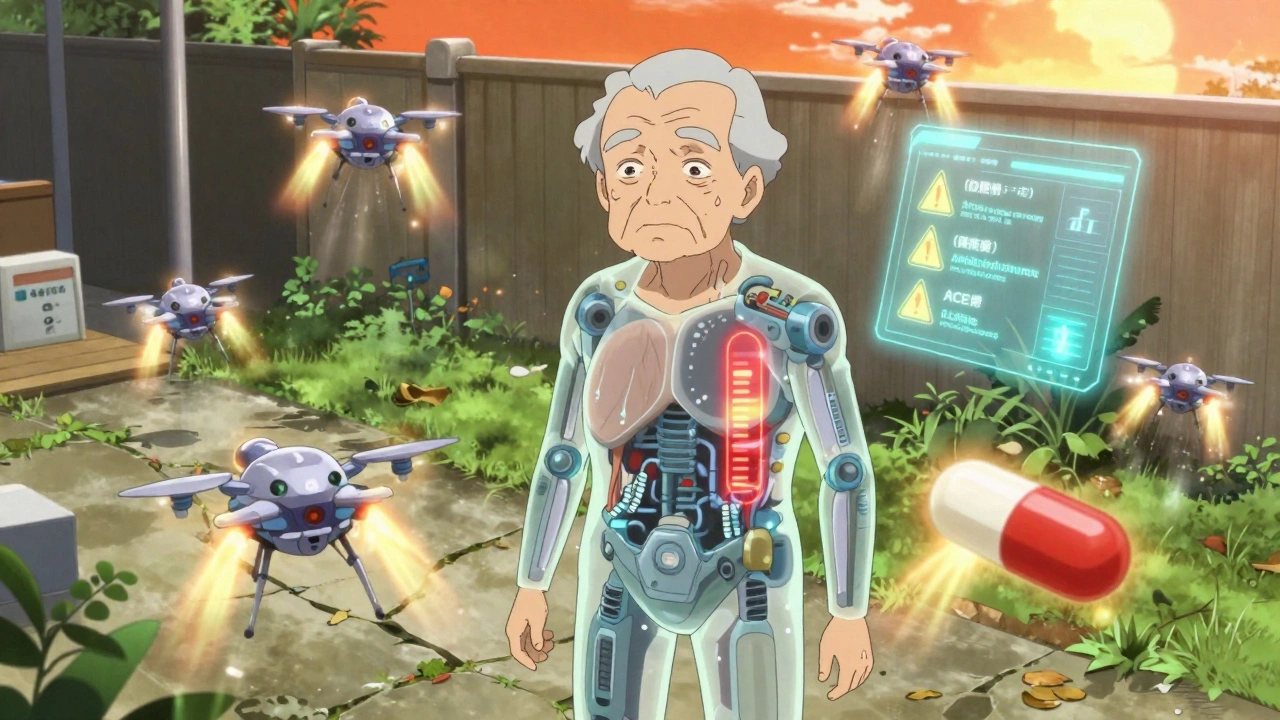
Not all drugs are equal when it comes to heat. Some are quietly dangerous. Diuretics like hydrochlorothiazide and furosemide, often called "water pills," make you pee more to lower blood pressure. But they also make you feel less thirsty-by 30% to 40%. That’s a deadly combo in hot weather. You’re losing fluids and your brain isn’t telling you to drink more.
ACE inhibitors and ARBs, used for high blood pressure and heart failure, also reduce thirst by about 25%. They’re not bad drugs-they save lives-but in heat, they need extra care. Then there are antipsychotics like quetiapine and clozapine, often given to seniors with dementia. These drugs interfere with the brain’s thermostat, raising core body temperature by 1.5°F to 2°F. That might sound small, but it’s enough to push someone into heat stroke.
Anticholinergics like diphenhydramine (Benadryl) and Tylenol PM are even sneakier. They block sweating-by 35% to 50%. No sweat means no cooling. Your body overheats from the inside out. And if you’re on more than one of these? The risk multiplies. A senior on a diuretic plus an ACE inhibitor is at triple the risk of low sodium, fainting, or falling. The CDC found that 22% of heat-related falls in seniors were tied to these drug combinations.
Even some antibiotics and antifungals make skin burn faster in the sun. Some seniors get sunburned after just 15 minutes outside-four to six times faster than normal. It’s not just about sunburn. It’s about your body’s ability to survive the day.
What to Do Before Summer Hits
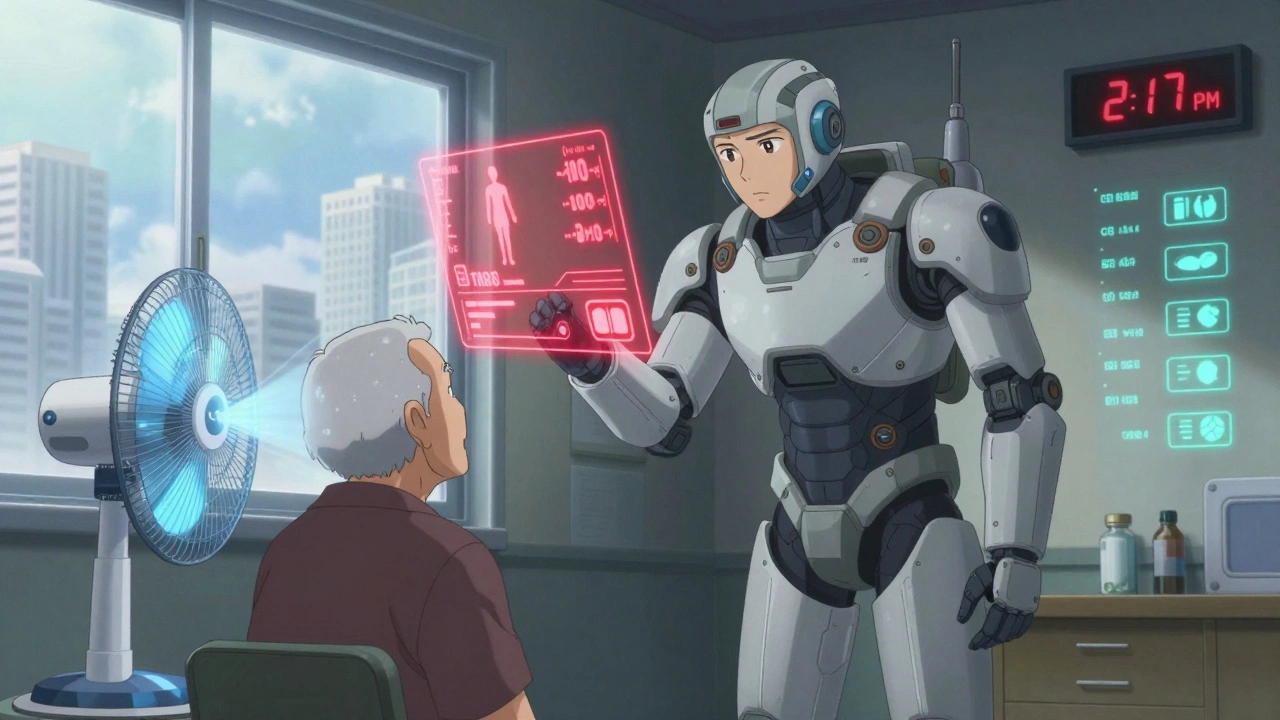
Waiting until it’s hot to check your meds is like checking your car’s oil after it overheats. The best time to act is in late spring. Sit down with your doctor or pharmacist and go through every pill, patch, and supplement. Ask: "Which of these make me more sensitive to heat?" Don’t assume your doctor knows all your meds. Many seniors see multiple specialists. One might prescribe a diuretic, another an anticholinergic, and neither talks to the other.
Ask for a heat risk checklist. The CDC’s Heat and Medication Risk Assessment Tool (HM-RAT), launched in 2023, helps doctors flag high-risk combinations. If you’re on two or more of the risky drugs listed above, your risk level is high. Don’t wait for an emergency. Get a plan now.
Some meds can be adjusted safely. For example, if you’re on a diuretic, your doctor might switch you to a lower dose or change the time you take it-like taking it in the morning instead of evening, so you’re not peeing all night and waking up dehydrated. Fluid restrictions for heart failure patients can sometimes be temporarily lifted during heat waves. Forty-three percent of those on fluid limits develop dangerous electrolyte drops when it’s hot. Your doctor can tell you if it’s safe to drink more.
Hydration That Actually Works
Drinking water isn’t enough if your body can’t hold onto the right balance of salts. The American Geriatrics Society recommends that seniors on diuretics drink electrolyte-enhanced beverages with 120-150 mg of sodium per 8 ounces. That’s not sports drinks with sugar-you want something like oral rehydration solutions or low-sugar electrolyte powders. Avoid caffeine and alcohol. Both increase urine output by 40% to 60%. A cup of coffee or a glass of wine might feel relaxing, but it’s pulling water out of your body when you need it most.
Drink even if you’re not thirsty. Your sense of thirst fades with age, especially if you’re on meds. Aim for 8-10 eight-ounce glasses of water daily during hot weather. Keep a water bottle with you at all times. Set phone alarms every two hours to drink. Don’t wait until you’re dry-mouthed or dizzy.
Stay Cool Without Air Conditioning
If you don’t have AC, you need a backup plan. The CDC says indoor temperatures should stay below 78°F (25.6°C). Without AC, that’s hard. Use fans with a bowl of ice in front of them. Close blinds during the day. Open windows at night if it’s cooler outside. Go to public places that are cool-libraries, malls, community centers. Many have cooling centers during heat waves.
Wear the right clothes. Light-colored, loose cotton lets air flow and helps sweat evaporate. Synthetic fabrics trap heat. Studies show cotton can lower your perceived temperature by 5°F to 7°F. Wear a wide-brimmed hat and UV-blocking sunglasses. Use broad-spectrum sunscreen with SPF 15 or higher. Reapply every two hours-or after sweating. Some medications make skin burn in minutes. Don’t risk it.
What Caregivers Must Do
If you’re caring for a senior, your role is critical. Don’t just check if they’re eating. Check if they’re drinking. Look for subtle signs: confusion, sluggishness, less talking, or not recognizing familiar people. The CDC says 78% of seniors show mental changes before physical symptoms like dizziness or nausea. That’s your early warning.
Use the "I’m OK" check-in system. Call or visit twice a day during heat waves. Ask: "How are you feeling?" Not just "Are you okay?"-that’s too vague. Say: "Do you feel dizzy? Hot? Nauseous? Thirsty?" Write down answers. If they say "I’m fine" but seem off, don’t ignore it. Call their doctor.
Plan outings around the heat. Avoid being outside between 10 a.m. and 4 p.m. Go shopping in the morning. Visit the library at noon. Even a few hours in a cool space can reset their body temperature.
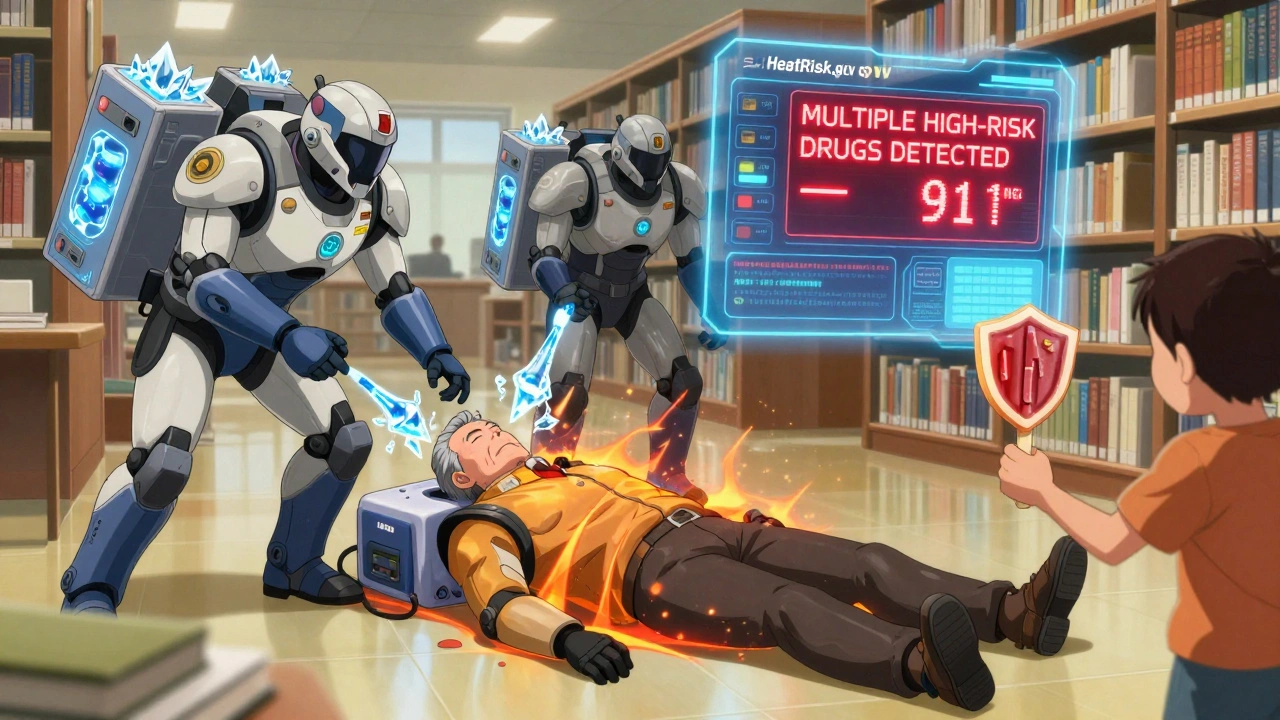
Warning Signs That Mean Call 911
Heat exhaustion looks like heavy sweating, headache, nausea, muscle cramps, dizziness, or fainting. But seniors often don’t sweat much-because of their meds. So if they’re hot, dry skin, confused, or have a fast pulse, that’s heat stroke. Body temperature above 103°F? That’s a medical emergency. One in two heat exhaustion cases turns into heat stroke within two to four hours if untreated.
Don’t wait. Move them to a cool place. Give them cool water if they’re alert. Sponge them with cool water. Put ice packs under arms and neck. But if they’re confused, vomiting, or unconscious-call 911 immediately. Don’t drive them yourself. Paramedics can start cooling and IV fluids on the way. For seniors with heart disease or high blood pressure, every minute counts.
The Future Is Here-And It’s Personalized
There’s new tech helping now. HeatRisk.gov, launched by the NIA and EPA, lets you enter your meds and your zip code. It gives you a daily heat risk score and alerts when it’s dangerous. Over 1.2 million seniors used it in 2023. Clinical trials are also testing a new "heat resilience" supplement designed for seniors on multiple meds. Early results show a 28% improvement in body temperature control.
Climate change means more extreme heat days. By 2050, we could see 50% more dangerous heat events. The CDC warns this will become one of the top five preventable causes of death in seniors. But you don’t have to wait for policy changes. The tools are here: medication reviews, hydration plans, cooling routines, and caregiver check-ins. Use them.
Can I stop my diuretic if it’s too hot?
Never stop or change a medication without talking to your doctor. Diuretics are often critical for heart or kidney health. But your doctor can adjust the dose, timing, or switch you to a different drug during hot months. Ask about temporary changes and how to monitor for side effects.
Do all seniors on blood pressure meds need to worry about heat?
Not all. Beta-blockers and calcium channel blockers generally don’t raise heat risk the way diuretics or ACE inhibitors do. But if you’re on two or more meds, the combination matters. A senior on a diuretic plus an ACE inhibitor is at much higher risk than someone on just one. Always review your full list with your pharmacist.
Is it safe to use a fan instead of AC?
Fans only move air-they don’t cool it. If the room is above 90°F, a fan won’t help and can actually make you hotter by blowing hot air over your skin. Use fans only when the air is cooler than your body temperature. For real cooling, seek air-conditioned spaces or use ice packs and cool cloths.
What if my senior won’t drink water?
Try alternatives: ice chips, popsicles made with electrolyte solution, broth, or water-rich fruits like watermelon and oranges. Add a splash of lemon or cucumber to water. Make it a habit-offer a glass every time they sit down. If they refuse fluids for over 12 hours, call their doctor. Dehydration can spiral fast.
Can heat make dementia symptoms worse?
Yes. Heat stress can cause sudden confusion, agitation, or withdrawal in seniors with dementia-even if they’re not overheated. This is often mistaken for a dementia flare-up. But it’s a heat reaction. Check their temperature, hydration, and meds. Cooling them down often reverses the confusion within hours.
What to Do Right Now
Today. Not tomorrow. Not next week. Open your medicine cabinet. Write down every pill, patch, and supplement. Look up each one on the CDC’s heat risk list. Call your doctor or pharmacist. Ask: "Which of these make me more vulnerable to heat?" Then make a plan: when to drink, where to go when it’s hot, who to call if something feels off. Keep that list on the fridge. Give a copy to your caregiver. Heat doesn’t wait. Neither should you.




Christian Landry
December 9, 2025 AT 18:58Katie Harrison
December 11, 2025 AT 06:09Michael Robinson
December 12, 2025 AT 14:11Kathy Haverly
December 13, 2025 AT 02:48Haley P Law
December 13, 2025 AT 04:46Andrea DeWinter
December 14, 2025 AT 02:54Steve Sullivan
December 14, 2025 AT 06:45George Taylor
December 16, 2025 AT 06:12ian septian
December 16, 2025 AT 20:08