Aripiprazole Neuropathy Dose Calculator
Dosing Information
This calculator helps determine appropriate starting dose and titration schedule for aripiprazole when used off-label for neuropathy pain. Based on the limited evidence from clinical studies.
Calculate Your Starting Dose
When nerve pain sticks around for months, many people start hunting for anything that might ease the burning, tingling, or shooting sensations. One drug that’s cropping up in online forums and a few research papers is aripiprazole. While it’s best known as an antipsychotic for schizophrenia and bipolar disorder, clinicians are beginning to wonder if it could also calm the nerves that cause neuropathy.
What is aripiprazole?
Aripiprazole is a dopamine partial agonist approved by the U.S. Food and Drug Administration (FDA) for treating schizophrenia, bipolar I disorder, and as an adjunct for major depressive disorder. In plain terms, it nudges dopamine receptors toward a balanced response rather than a full‑on or full‑off signal. This “partial agonist” property is why it tends to cause fewer side‑effects like weight gain compared with older antipsychotics.
Understanding neuropathy
Neuropathy is a blanket term for damage to peripheral nerves. The most common sub‑type is Peripheral Neuropathy, where the nerves outside the brain and spinal cord are affected. When diabetes is the culprit, it’s called Diabetic Neuropathy, which accounts for roughly 60‑70% of all cases in the United States. Symptoms range from mild tingling to intense, stabbing pain that can cripple daily activities.
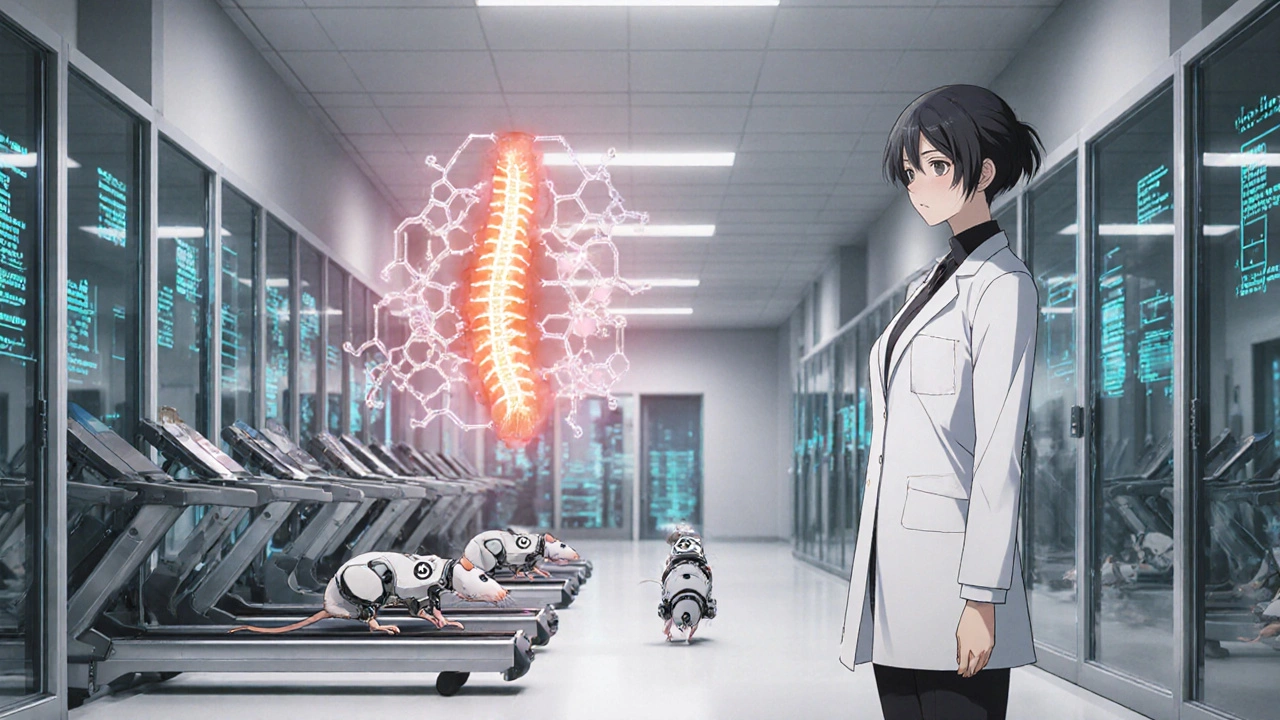
How could aripiprazole influence nerve pain?
Traditional neuropathy meds - gabapentin, pregabalin, duloxetine - work by damping nerve excitability or boosting serotonin/norepinephrine pathways. Aripiprazole, on the other hand, modulates dopamine. Recent animal studies suggest that dopamine signaling can affect the way pain signals are processed in the spinal cord. A 2023 pre‑clinical trial on rodents showed that a dopamine‑partial agonist reduced mechanical allodynia by about 30% compared with control groups.
Clinical evidence: What do human studies say?
Human data are still sparse, but a handful of small‑scale investigations provide clues:
- Open‑label pilot (2022): 15 patients with refractory diabetic neuropathy added low‑dose aripiprazole (2‑5 mg daily) to their existing gabapentin regimen. After 12 weeks, 9 reported at least a 20% drop in pain scores on the Visual Analog Scale (VAS).
- Retrospective chart review (2023): Analyzed 78 patients who were prescribed aripiprazole for mood disorders and also suffered from neuropathic pain. Approximately 42% noted a subjective improvement, especially those on 5‑10 mg doses.
- Phase‑II randomized trial (ongoing, 2025): Recruiting 120 participants with chemotherapy‑induced peripheral neuropathy to compare aripiprazole 5 mg vs placebo. Early interim data (released at a conference) suggest a modest but statistically significant reduction in pain intensity.
While promising, these studies share limitations: small sample sizes, short follow‑up, and many participants continued other neuropathy meds. The evidence is far from conclusive, which is why clinicians label the use as “off‑label.”
Off‑label prescribing: What you need to know
Off‑label doesn’t mean illegal; it simply means the drug’s use hasn’t been formally approved for that condition by the FDA. Physicians can prescribe it if they believe the potential benefit outweighs the risk and if they discuss the rationale with the patient. Important steps include:
- Confirm an accurate diagnosis of neuropathy and rule out reversible causes.
- Document prior attempts with standard agents (gabapentin, duloxetine, topical capsacin).
- Explain that evidence is limited and side‑effects are possible.
- Start with the lowest effective dose (often 2 mg daily) and titrate slowly.
- Schedule regular follow‑ups to assess pain scores, mood, and any adverse events.
Potential side effects and cautions
Because aripiprazole acts on dopamine, it can trigger a different side‑effect profile than typical neuropathy drugs:
- Akathisia (inner restlessness) - more common at higher doses.
- Insomnia or mild agitation - especially when taken later in the day.
- Metabolic changes: modest weight gain, slight rise in fasting glucose (relevant for diabetic patients).
- Extrapyramidal symptoms (rare at low doses).
- Potential drug‑drug interactions with CYP2D6 inhibitors (e.g., fluoxetine).
Patients with a history of cardiac arrhythmia should have a baseline ECG, as aripiprazole can cause QT‑interval changes in susceptible individuals.
How does aripiprazole stack up against standard neuropathy meds?
| Drug | Primary Mechanism | FDA‑Approved Indication for Pain | Evidence for Nerve Pain | Typical Dose for Pain | Common Side Effects |
|---|---|---|---|---|---|
| Aripiprazole | Dopamine partial agonist | No (off‑label) | Small pilots, ongoing Phase‑II | 2‑10 mg daily | Akathisia, insomnia, metabolic shifts |
| Gabapentin | Calcium channel α2‑δ subunit binder | Yes (post‑herpetic neuralgia) | Robust, multiple RCTs | 300‑1800 mg TID | Drowsiness, edema, dizziness |
| Pregabalin | Similar to gabapentin, higher potency | Yes (diabetic neuropathy, post‑herpetic) | Strong RCT evidence | 150‑600 mg BID | Dizziness, weight gain, peripheral edema |
| Duloxetine | Serotonin‑norepinephrine reuptake inhibitor | Yes (diabetic peripheral neuropathy) | Solid, multiple meta‑analyses | 60‑120 mg daily | Nausea, dry mouth, fatigue |
From the table you can see that aripiprazole’s evidence base is still thin, but its side‑effect profile at low doses can be more tolerable for some patients who can’t handle the sedation from gabapentin or the nausea from duloxetine.
Practical checklist for patients considering aripiprazole
- Verify that you have a confirmed neuropathy diagnosis.
- Discuss any existing psychiatric conditions - aripiprazole may also help mood, which can be a bonus.
- Ask your doctor about starting at 2 mg and how to titrate.
- Track pain daily using a simple 0‑10 scale; note any new restlessness or sleep issues.
- Schedule a follow‑up at 4 weeks to review benefits vs. side‑effects.
- Never stop abruptly; taper if you’ve been on it for more than a month.
Bottom line: Is aripiprazole worth a try?
If you’ve exhausted first‑line agents and still grapple with burning nerve pain, a low‑dose trial of aripiprazole under a physician’s supervision is a reasonable next step. The drug isn’t a miracle cure, but with careful dosing it might tip the balance toward less pain and better quality of life. Always weigh the limited research against potential side‑effects and keep an open line of communication with your healthcare team.
Can aripiprazole be taken with other neuropathy medications?
Yes, many clinicians add aripiprazole to existing regimens like gabapentin or duloxetine. The key is to start at a low dose and watch for additive side‑effects such as dizziness or increased sedation.
How quickly can I expect pain relief?
Most small studies report noticeable changes after 4‑6 weeks of consistent dosing, but individual responses vary. Some patients feel better within two weeks, while others need a full 12‑week trial.
Is aripiprazole safe for people with diabetes?
Generally safe at low doses, but watch for modest increases in blood glucose. Regular monitoring and coordination with your endocrinologist are advisable.
What are the most common side effects when used for nerve pain?
The most frequent are akathisia (inner restlessness), insomnia, and mild weight gain. These tend to be dose‑related, so staying at the lowest effective dose can mitigate them.
Should I stop aripiprazole if I feel better?
Don’t stop abruptly. Gradually taper under medical guidance to avoid withdrawal or rebound symptoms.




laura wood
October 20, 2025 AT 14:35Reading about aripiprazole's off‑label journey into neuropathy care really hits home for many of us who have felt the relentless sting of nerve pain. I remember the first time I was told my diabetic neuropathy was "hard to manage" and the frustration that followed. The idea of repurposing a well‑known antipsychotic feels both innovative and a little daring, especially when conventional meds leave us drowsy or nauseous. The article does a solid job laying out the mechanisms, showing how dopamine modulation might calm hyper‑active pain pathways in the spinal cord. It’s fascinating that animal studies reported a 30% reduction in mechanical allodynia, suggesting a real physiological effect. Human data, though small, are encouraging – the 2022 pilot where nine out of fifteen patients reported meaningful pain relief shows promise. I think the key is the low‑dose approach, starting at 2 mg, which seems to keep side‑effects at bay while still offering a therapeutic window. Patient vigilance is essential; tracking VAS scores daily can reveal subtle improvements or early signs of akathisia. Collaboration with a prescriber who understands both psychiatric and pain management realms makes the off‑label use safer. For anyone juggling diabetes, keeping an eye on glucose levels while on aripiprazole is prudent, given the modest metabolic shifts noted. The checklist at the end of the article is a practical tool that I would hand to anyone considering this option. Overall, while we await larger trials, the combination of scientific rationale and patient anecdotes gives a hopeful glimpse into another arsenal piece for chronic nerve pain.
JessicaAnn Sutton
October 28, 2025 AT 16:15The manuscript, while informative, suffers from an overreliance on anecdotal evidence and underpowered studies. A rigorous meta‑analysis is conspicuously absent, leaving the reader with speculative conclusions. Moreover, the presentation of dosage ranges lacks the precision required for clinical guidance. The authors ought to delineate the pharmacokinetic profile of aripiprazole in neuropathic cohorts, not merely cite a handful of open‑label pilots. Such omissions reduce the utility of the piece for evidence‑based practitioners.
Israel Emory
November 5, 2025 AT 18:55Listen up, folks! The data on aripiprazole for nerve pain is not a myth, it’s a developing reality; we have rodent models showing reduced allodynia, we have human pilots with modest success, and we have an ongoing Phase‑II trial that promises real numbers. Yes, the sample sizes are small-yes, the follow‑up is short-BUT the trend is unmistakable. If you dismiss it because “the evidence isn’t perfect,” you’re ignoring the very nature of medical progress, which thrives on incremental innovation! So, keep an open mind, but also demand rigorous trials.
Sebastian Green
November 13, 2025 AT 21:35I’ve tried the low‑dose regimen myself, and the gradual reduction in tingling was noticeable after about five weeks. The key for me was pairing it with my existing gabapentin and monitoring any restlessness. It didn’t erase the pain entirely, but it gave me breathing room from the constant burning.
Wesley Humble
November 22, 2025 AT 00:15From a pharmacological standpoint, the dopamine partial agonism of aripiprazole offers a novel mechanism distinct from the serotonin‑norepinephrine reuptake inhibition of duloxetine. Theoretically, this could complement existing regimens, reducing dose‑dependent side‑effects such as sedation. However, clinicians must remain vigilant for akathisia, especially at doses exceeding 5 mg. 📈📊 In summary, while the empirical evidence remains preliminary, the mechanistic rationale warrants cautious optimism.
jessie cole
November 30, 2025 AT 02:55Friends, let me tell you a story: imagine standing in a storm of fire, every step a blaze. That is what chronic neuropathic pain feels like. Now picture a gentle rain-just a light drizzle-softening the flames. Low‑dose aripiprazole can be that drizzle, easing the intensity without drowning you in sedation. Start low, stay consistent, and always communicate with your doctor. You deserve relief, and sometimes the answer lies in a medication you never considered.
Vijaypal Yadav
December 8, 2025 AT 05:35The pharmacodynamics of aripiprazole suggest a ceiling effect at low milligram doses, which aligns with the observed safety profile. Interaction with CYP2D6 substrates should be screened, particularly fluoxetine, to avoid plasma level spikes. Clinical monitoring intervals of four weeks are reasonable to assess efficacy and tolerability.
Deja Scott
December 16, 2025 AT 08:15This approach could be a viable option for patients with refractory neuropathy.
Natalie Morgan
December 24, 2025 AT 10:55Exploring new avenues shows courage-keep tracking your pain scores and share progress with your care team.
Mahesh Upadhyay
January 1, 2026 AT 13:35While the temptation to grasp at any potential remedy is strong, we must not abandon rigor; short studies cannot justify widespread use, yet dismissing every novel hypothesis would betray scientific curiosity. Balance, therefore, is the true virtue.