Why Your Go-Bag Needs More Than Just Water and Flashlights
If you’ve ever been caught in a power outage, flood, or wildfire, you know how fast normal life falls apart. You grab your phone, your wallet, maybe your pet. But what about your meds? If you take daily pills for high blood pressure, diabetes, asthma, or depression, skipping even one dose can land you in the ER-or worse. During emergencies, pharmacies close, power goes out, and roads get blocked. That’s when your go-bag isn’t just helpful-it’s life-saving.
According to the CDC, 89% of Americans over 65 take at least one prescription medication. But only 22% of households have a proper emergency supply on hand. And it’s not just seniors. One in five adults under 35 has a chronic condition requiring daily meds. If you’re one of them, waiting until the storm hits to think about your pills is a dangerous gamble.
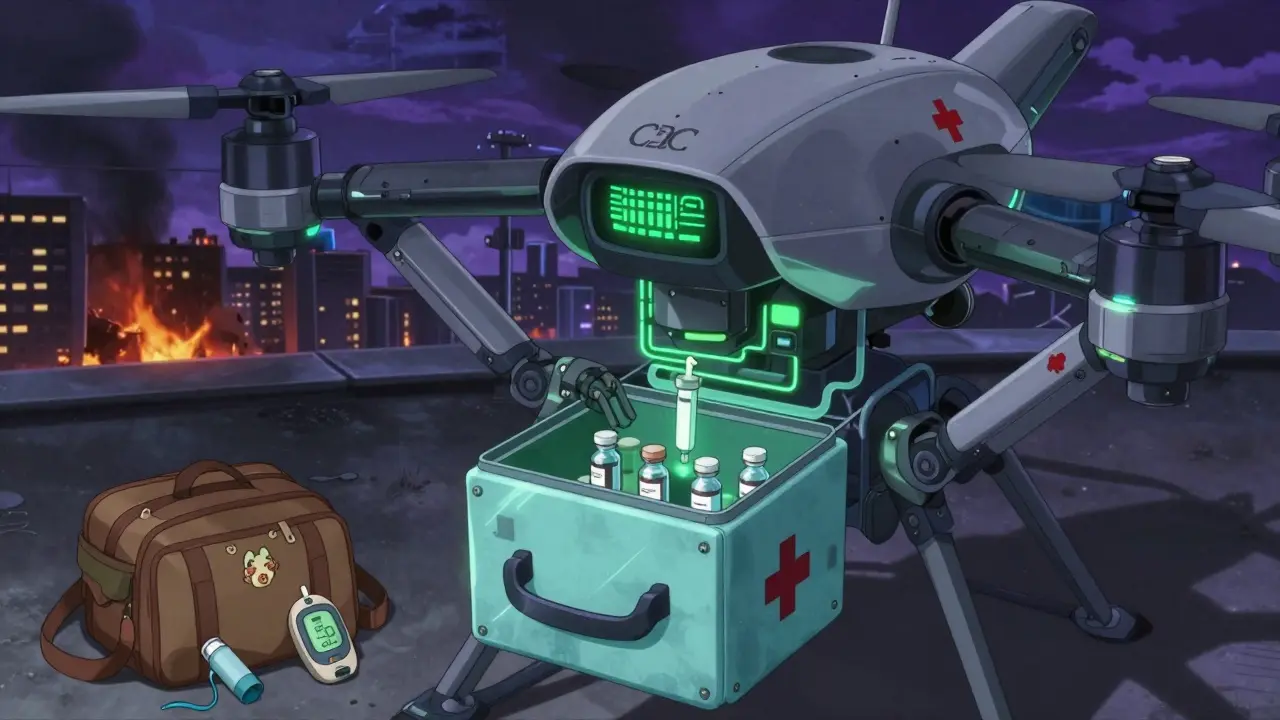
What Exactly Goes in a Medication Go-Bag?
A medication go-bag isn’t just a shoebox full of bottles. It’s a carefully organized system designed to keep you safe when you can’t get to your medicine cabinet. The American Red Cross recommends a minimum seven-day supply, but experts like Alert San Diego and the CDC now advise two weeks. Why? Because disasters don’t always end in three days. Hurricane Ida left people stranded for over a week. California wildfires forced evacuations lasting 10+ days. You need enough to cover the worst-case scenario.
Here’s what you actually need to pack:
- At least a 14-day supply of every prescription medication you take daily. Don’t guess-count your pills. If your last refill was three weeks ago, you’re already behind.
- Over-the-counter essentials: Pain relievers (ibuprofen, acetaminophen), antihistamines, anti-diarrheal meds, and antacids. These aren’t optional. Fever, allergies, or stomach bugs can turn dangerous without treatment.
- Medical devices: Inhalers, epinephrine auto-injectors, glucose monitors, insulin pumps. These aren’t just pills-they’re lifelines.
- Cooling solutions for temperature-sensitive drugs: Insulin, certain biologics, and some antibiotics need to stay between 36°F and 86°F. A regular bag won’t cut it. Use an FDA-cleared cooling case like the Frio Wallet or MedAngel ONE, which alerts you via phone if temps rise too high.
Documentation: The Most Overlooked Part
Imagine being rushed to a hospital after a crash. You can’t speak. You don’t remember your meds. The ER staff has to guess. That’s why your go-bag needs more than pills-it needs paper.
Include a waterproof, zip-seal pouch with:
- A printed list of every medication: name, dosage, frequency, reason for taking it (e.g., "Lisinopril 10mg once daily for high blood pressure").
- Your allergies and past reactions (e.g., "Allergic to penicillin-rash and swelling").
- Your primary doctor’s name and phone number.
- Your insurance card and a copy of your ID.
- Any advance directives or living wills if you have them.
Westchester County Emergency Services says this info is critical. One Redditor, SurvivorMom, credited her printed list with preventing a dangerous drug interaction during a flash flood evacuation. Emergency responders don’t have time to call your pharmacy. They need the facts in their hands.
Storage and Maintenance: Don’t Let Your Meds Go Bad
Packing your meds is only half the battle. If they’re exposed to heat, moisture, or sunlight, they can lose potency-or become toxic. Epinephrine auto-injectors, for example, degrade quickly after expiration. A 2023 study found that insulin exposed to 95°F for 48 hours lost up to 30% of its effectiveness.
Store your go-bag:
- In a water-resistant, durable container (like a sealed plastic bin or a specialized emergency bag).
- In a cool, dry spot-like a high shelf in your bedroom closet. Avoid the bathroom (humidity) or the car (heat).
- Out of reach of kids and pets.
Check your bag every six months. Set a calendar reminder for June 1 and December 1. Toss expired pills. Replace anything you’ve used. Rotate your supply so you’re always using the oldest meds first. If you refill your prescriptions on the first day you’re eligible (not the last), you’ll always have a fresh batch to swap in.
Special Cases: Insulin, Biologics, and Complex Regimens
If you’re on insulin, you’re not just managing diabetes-you’re managing survival. The American Diabetes Association estimates 1.2 million Americans rely on temperature-sensitive biologics. Most go-bags fail them.
Here’s what you need to do:
- Always carry insulin in a cooling case. The Frio Wallet, tested by Consumer Reports, keeps insulin below 86°F for 48 hours without ice.
- Bring extra syringes, alcohol wipes, and a backup glucose meter with extra batteries.
- Know your pharmacy’s emergency refill policy. In 42 states, pharmacists can give you a 30-day emergency supply without a new prescription during a declared disaster.
- Ask your doctor for a 90-day supply instead of 30. Many insurers allow this for chronic conditions.
Same goes for injectables like Humira, Enbrel, or other biologics. These can’t be refrigerated in a regular cooler for long. The MedAngel ONE sensor (FDA-cleared in April 2023) connects to your phone and sends alerts if your meds get too hot or cold. It’s not cheap, but for some, it’s the only way to stay safe.
What to Avoid
People make the same mistakes over and over:
- Keeping meds in original bottles without labels. If the label peels off, you’re stuck. Keep bottles with clear, readable labels.
- Using pill organizers as your main storage. They’re great for daily use, but not for emergencies. They don’t protect from heat, moisture, or damage. Use them as a daily dispenser, not your go-bag.
- Waiting until a storm is coming. If you’re told to evacuate, you won’t have time to fill prescriptions. Start now.
- Assuming hospitals will give you your meds. The CDC says 38% of ER visits during disasters are due to interrupted meds. Hospitals aren’t pharmacies. They’ll treat you, but they won’t hand out your regular prescriptions.

Who Needs This Most?
You might think this is only for older adults. But it’s not.
People with:
- Heart disease (beta-blockers, blood thinners)
- Diabetes (insulin, metformin)
- Asthma or COPD (inhalers, nebulizers)
- Seizure disorders (anticonvulsants)
- Mental health conditions (antidepressants, anti-anxiety meds)
- Autoimmune diseases (immunosuppressants)
…are at highest risk. The CDC reports that 157 million Americans have chronic conditions. That’s nearly half the population. If you take meds daily, you’re in this group.
And don’t forget kids. AdventHealth Children’s Hospital says parents often forget their child’s asthma inhaler or seizure meds during evacuations. Make a separate go-bag for each child. Include their school nurse’s contact info.
How to Get Started Today
Don’t wait for a warning siren. Start now. Here’s your 5-step plan:
- Inventory your meds. Write down every pill, injection, and device you use daily. Include OTC stuff.
- Call your pharmacy. Ask if you can get a 90-day supply. Most insurers allow it for chronic conditions.
- Buy a go-bag. Look for one with compartments, waterproof lining, and a handle. No backpacks with zippers that break.
- Fill it. Put in 14 days of meds, cooling devices if needed, and your printed medical info.
- Set a reminder. Check it every six months. Rotate supplies. Toss expired stuff.
It takes two or three tries to get it right. That’s normal. The goal isn’t perfection-it’s protection.
Final Thought: This Isn’t Optional
Emergency kits for food, water, and flashlights are common. But meds? They’re often ignored. And that’s deadly. During Hurricane Ida, 23% of evacuees ran out of medication. Cardiovascular drugs were the most common gap. People died because they skipped a dose.
You can’t control when the next disaster hits. But you can control whether your meds are ready. Your go-bag isn’t a luxury. It’s your insurance policy. And right now, you’re uninsured.
Can I just keep my meds in my car or garage?
No. Cars and garages get too hot in summer and too cold in winter. Medications like insulin, epinephrine, and some antibiotics can break down quickly in extreme temperatures. Store your go-bag in a cool, dry place inside your home-like a closet shelf. Avoid the bathroom, kitchen, or basement.
What if I can’t afford a 14-day supply?
Talk to your pharmacist. In 42 states, pharmacists can give you a 30-day emergency supply without a new prescription during a declared emergency. Ask if your insurance allows 90-day fills for chronic conditions. Some pharmacies offer discount programs or patient assistance plans. Even a 7-day supply is better than nothing-but aim for two weeks.
Do I need to keep my meds in original bottles?
Yes. Original bottles have the pharmacy label with your name, drug name, dosage, and expiration date. If you transfer pills to a pill organizer, keep the original bottles in your go-bag. Emergency responders need to verify what you’re taking.
How often should I check my go-bag?
Every six months. Set a reminder for January 1 and July 1. Check expiration dates. Replace anything you’ve used. Swap out old meds for fresh ones. If your insulin is expired, toss it. Don’t risk it.
What if I use injectables like insulin or epinephrine?
You need cooling solutions. Use a Frio Wallet or MedAngel ONE sensor to keep insulin at safe temperatures. Always carry extra syringes, alcohol wipes, and batteries for your glucose monitor. Epinephrine auto-injectors expire-replace them before the date. Keep at least two on hand.




Wren Hamley
January 4, 2026 AT 06:48Kerry Howarth
January 4, 2026 AT 17:55Joy F
January 6, 2026 AT 08:30Shruti Badhwar
January 7, 2026 AT 03:43Liam Tanner
January 8, 2026 AT 23:54Palesa Makuru
January 9, 2026 AT 13:44Lori Jackson
January 10, 2026 AT 21:51Sarah Little
January 10, 2026 AT 23:10innocent massawe
January 12, 2026 AT 09:50Ian Ring
January 13, 2026 AT 10:01erica yabut
January 15, 2026 AT 04:28Tru Vista
January 16, 2026 AT 21:26Vincent Sunio
January 17, 2026 AT 01:21JUNE OHM
January 17, 2026 AT 13:39Philip Leth
January 18, 2026 AT 05:31