When someone hears the word brain tumor, fear often comes before facts. But not all brain tumors are the same. Some grow slowly and stay contained. Others spread fast, invade healthy tissue, and demand aggressive treatment. Understanding the difference isn’t just academic-it directly shapes survival, quality of life, and treatment choices. The key lies in three things: type, grade, and how treatments are combined.
What Are the Main Types of Brain Tumors?
Brain tumors aren’t one disease. They’re dozens, each starting from different cells in the brain or surrounding tissues. The most common types fall into three groups: gliomas, meningiomas, and others like pituitary tumors or schwannomas.
Gliomas come from glial cells-the brain’s support system. These include astrocytomas, oligodendrogliomas, and ependymomas. Among them, glioblastoma is the most aggressive and most common malignant brain tumor in adults. It makes up more than half of all gliomas. Then there are meningiomas, which form in the membranes covering the brain and spinal cord. These are often benign but can still cause serious problems by pressing on brain tissue. About 30% of all primary brain tumors are meningiomas.
What sets these apart isn’t just where they grow, but what they’re made of at the molecular level. That’s where the 2021 WHO Classification of CNS Tumors changed everything. Before, doctors looked only at how cells looked under a microscope. Now, they test for specific gene changes. For example, an astrocytoma with an IDH mutation behaves very differently than one without it-even if they look identical under the lens. That’s why two grade 2 tumors can have wildly different outcomes.
Understanding Tumor Grades: From 1 to 4
Grade tells you how fast a tumor is likely to grow and how dangerous it is. The World Health Organization uses a scale from 1 to 4. Grade 1 is the slowest, grade 4 the fastest.
Grade 1 tumors, like pilocytic astrocytoma, look almost normal under the microscope. They grow slowly, have clear borders, and rarely spread. Many can be cured with surgery alone. Grade 2 tumors, such as diffuse astrocytoma, are trickier. Their cells look slightly abnormal, and they creep into healthy brain tissue like roots. They may stay quiet for years, but they often come back as higher-grade tumors later.
Grade 3 tumors are called anaplastic. Cells multiply quickly, invade nearby areas, and rarely stay contained. An anaplastic astrocytoma or anaplastic oligodendroglioma falls here. These need radiation and chemotherapy after surgery. Grade 4 is the worst. Glioblastoma (IDH-wildtype) is the classic example. These tumors grow so fast they starve their own center, creating dead zones (necrosis). They also build new blood vessels to feed themselves. Even with treatment, median survival is around 14.6 months.
But here’s the twist: not all grade 4 tumors are the same. An IDH-mutant glioblastoma-yes, it’s still grade 4-can live for over 31 months on average. That’s more than double the survival of its IDH-wildtype cousin. Molecular testing isn’t optional anymore. It’s the difference between guessing and knowing.
How Grading Changed in 2021 (WHO CNS5)
The 2021 update to the WHO classification didn’t just tweak a few labels. It rewrote the rulebook. Before, a tumor’s grade was based only on how it looked. Now, molecular markers are required for diagnosis. You can’t call something a glioblastoma unless you’ve tested for IDH status and 1p/19q codeletion.
One major change was moving from Roman numerals (I, II, III, IV) to Arabic numbers (1, 2, 3, 4). Why? Because tumor behavior isn’t a series of boxes-it’s a spectrum. Arabic numbers better reflect that. Another big shift was the move to “within-tumor-type” grading. Before, all anaplastic astrocytomas were grade 3. Now, you can have a grade 2, 3, or 4 astrocytoma depending on molecular features. That means two people with the same tumor name can have very different prognoses.
For oligodendrogliomas, the rules are tighter. They only exist as grade 2 or 3-and only if they have both an IDH mutation and 1p/19q codeletion. If they’re missing one, they’re reclassified as something else. Meningiomas still use a 1-3 scale, but even there, molecular markers like TERT promoter mutations now help predict recurrence risk.
Doctors who used to rely on histology alone now need to interpret genetic reports. A 2022 study found pathologists needed to review nearly 18 cases before they could accurately apply the new system. It’s not easy. But the payoff? Better predictions, fewer misdiagnoses, and smarter treatment plans.
How Treatment Is Changing: Multimodal Therapy
There’s no single cure for brain tumors. Treatment is a layered approach-surgery, radiation, chemo, targeted drugs, and sometimes immunotherapy-all used together. That’s multimodal therapy.
Surgery comes first when possible. The goal isn’t always to remove everything-sometimes it’s to reduce pressure, get tissue for testing, or make other treatments more effective. For low-grade tumors, surgery alone might be enough. For high-grade tumors, it’s just step one.
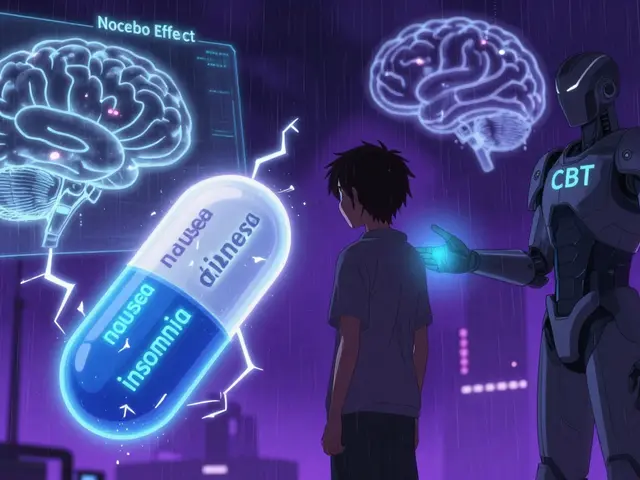
Radiation therapy follows, especially for grades 3 and 4. It’s targeted to avoid healthy brain tissue, but side effects like fatigue, memory issues, and hair loss are common. Chemotherapy, usually temozolomide, is often given at the same time and after radiation. It works best when the MGMT gene promoter is methylated-a molecular marker that makes tumor cells more vulnerable to the drug.
But the biggest breakthrough in recent years is targeted therapy. In June 2023, the FDA approved vorasidenib for grade 2 gliomas with IDH mutations. In the INDIGO trial, patients on vorasidenib had a median progression-free survival of 27.7 months-more than double the 11.1 months seen with placebo. That’s not just an extension of life. It’s a delay in disability. For many, it means avoiding radiation for years.
Other drugs are in trials. The CODEL trial is testing a combo of chemotherapy for oligodendrogliomas. Liquid biopsies-testing tumor DNA in spinal fluid-are showing 89% accuracy in detecting recurrence before symptoms appear. That could change how often people need MRIs.
What Patients Are Really Facing
Behind the numbers are real people. A 32-year-old diagnosed with a grade 2 oligodendroglioma was told she had 72 hours to decide whether to freeze her eggs before surgery. Another man, told he had glioblastoma, learned his tumor had an IDH mutation-and suddenly, his prognosis wasn’t just months, but years.
But delays are still common. A 2022 survey found 68% of patients waited more than 8 weeks for a diagnosis. Those with low-grade tumors waited longer-14 weeks on average. Why? Because low-grade tumors often look like benign cysts on scans. They’re easy to miss. And when they’re misdiagnosed, treatment is delayed.
There’s also confusion about what grades mean. A 2022 study found 42% of patients thought a grade 2 tumor meant a 20% survival rate. It doesn’t. Grade 2 means slow growth. Many live for decades. But without proper counseling, fear replaces understanding.
Cost is another barrier. Molecular testing adds $3,200 to $5,800 to the diagnostic bill. Insurance doesn’t always cover it. And not every hospital has the labs or pathologists trained to do it right. That creates a gap between those who get precision care and those who don’t.

What’s Next for Brain Tumor Care
The future is personal. Treatment is moving away from one-size-fits-all. Instead, it’s built on the tumor’s DNA, not just its shape. Clinical trials are now designed around molecular subtypes, not just location or grade.
Researchers are testing vaccines that train the immune system to attack IDH-mutant cells. Others are exploring drugs that block the metabolic changes tumors use to survive. And AI is being trained to spot tumor patterns on MRI scans faster than human eyes.
The WHO system has been updated five times since 1979. Each time, it got more accurate. The next update won’t be about adding more grades. It’ll be about integrating real-time data-like blood or spinal fluid tests-into daily decisions. That’s the next leap: turning a static diagnosis into a living, evolving plan.
For now, the message is clear: Know your tumor’s type. Know its grade. Know its mutations. And don’t accept a treatment plan without molecular confirmation. The right combination of surgery, radiation, chemo, and targeted drugs can turn a death sentence into a manageable condition. And that’s progress.
What’s the difference between a low-grade and high-grade brain tumor?
Low-grade tumors (grades 1-2) grow slowly, have clear borders, and rarely spread. They’re often treatable with surgery alone. High-grade tumors (grades 3-4) grow fast, invade healthy brain tissue, and almost always come back. They require radiation, chemotherapy, and sometimes targeted drugs. Grade 4 tumors, like glioblastoma, are the most aggressive and have the poorest survival rates-unless they have an IDH mutation, which can double survival time.
Can a grade 2 brain tumor become grade 4?
Yes. Grade 2 tumors like diffuse astrocytoma can evolve into higher grades over time, sometimes over years, sometimes within months. That’s why regular MRIs are critical-even if you feel fine. Molecular testing helps predict this risk. Tumors with certain gene changes (like CDKN2A deletion) are more likely to progress. Monitoring isn’t just precautionary-it’s life-saving.
Why does molecular testing matter so much?
Two tumors that look identical under a microscope can behave completely differently. An IDH-mutant glioblastoma (grade 4) survives over 31 months on average. An IDH-wildtype one? Just 14.6 months. Testing for IDH, 1p/19q codeletion, and MGMT methylation tells doctors which drugs will work, how aggressive to be, and what to expect. Skipping molecular testing is like driving blindfolded.
Is surgery always the first step?
Not always. For small, slow-growing tumors in safe areas, doctors may monitor with scans first. For tumors near critical brain areas (like the motor cortex), removing too much can cause paralysis or speech loss. In those cases, biopsy + radiation or targeted drugs may come before major surgery. The goal isn’t to remove everything-it’s to preserve function while controlling growth.
What’s the newest treatment for grade 2 gliomas?
Vorasidenib, approved by the FDA in June 2023, is the first drug specifically for IDH-mutant grade 2 gliomas. In the INDIGO trial, it delayed tumor growth for 27.7 months-more than double the placebo group. It’s taken orally, has fewer side effects than chemo, and can delay the need for radiation or surgery for years. It’s not a cure, but it’s a major step toward turning a brain tumor into a chronic condition.
How long does it take to get a final brain tumor diagnosis?
It usually takes 7 to 10 business days after biopsy for a full diagnosis. That’s because molecular testing (for IDH, 1p/19q, MGMT) must be done alongside histology. Some hospitals with fast-track labs can deliver results in 48 hours using new IDH antibody tests, but most still need over a week. Waiting is stressful, but rushing leads to errors. Accuracy matters more than speed.
Are brain tumors hereditary?
Most brain tumors are not inherited. Less than 5% are linked to genetic syndromes like neurofibromatosis, Li-Fraumeni, or Lynch syndrome. If you have a family history of multiple cancers, especially at young ages, genetic counseling may be helpful. But for the vast majority, brain tumors arise from random mutations-not genes passed down from parents.
What You Should Do Now
If you or someone you know has been diagnosed, ask these three questions: What’s the exact tumor type? What’s the molecular profile? And what’s the treatment plan based on? Don’t accept a grade without an IDH test. Don’t agree to radiation without knowing if MGMT is methylated. And don’t skip second opinions-especially at major cancer centers with neuro-oncology programs.
The science has moved fast. Your treatment should too. Knowledge isn’t just power-it’s time. And time is the one thing no one wants to lose.


Paige Shipe
December 29, 2025 AT 12:15Brain tumors aren’t just tumors-they’re genetic puzzles with survival odds written in DNA. The 2021 WHO update wasn’t a tweak, it was a revolution. IDH status alone can double your life expectancy. If your doctor hasn’t tested for it, demand it. No excuses. This isn’t sci-fi-it’s standard of care now.
Tamar Dunlop
December 29, 2025 AT 12:55It is with profound reverence that I acknowledge the quiet courage of those navigating this labyrinth of molecular complexity. To receive a diagnosis-then to be told, ‘Your tumor’s DNA holds the key to your future’-is both terrifying and strangely beautiful. Science has begun to listen to the whisper of our cells, and for that, we must pause, breathe, and give thanks.
David Chase
December 31, 2025 AT 11:08USA still leads in neuro-oncology, no cap. 🇺🇸 Vorasidenib? FDA-approved and American-made. Meanwhile, Europe’s still arguing over whether to spell ‘tumor’ with an ‘o’ or ‘u’. 😒 MGMT methylation? If you don’t test it, you’re just guessing. And guessing kills. Period. 🚫🧠
Emma Duquemin
January 1, 2026 AT 00:02Let me tell you-this isn’t just medicine, it’s a revolution in slow motion. Imagine a world where your tumor’s DNA writes your treatment plan instead of a doctor’s hunch. Vorasidenib? It’s not a miracle drug-it’s a pause button on the clock. For someone with a grade 2 glioma, that’s years of birthdays, graduations, late-night laughs. This is hope with a molecular address.
And the fact that we’re now using spinal fluid to detect recurrence before symptoms hit? That’s like having a smoke alarm for cancer. No more waiting until you’re dizzy or blind. We’re catching it before it whispers-before it screams.
But here’s the kicker: most patients don’t even know to ask for molecular testing. They think ‘grade 2’ means ‘it’s not that bad.’ Nope. It means ‘it’s quietly plotting.’ And if you skip the IDH test? You’re flying blind in a storm with no radar.
And cost? $5,800? That’s less than a new car. But insurance? Sometimes they treat genetic testing like a luxury spa day. It’s not. It’s survival. Period.
My cousin got diagnosed with an IDH-mutant glioma. Two years ago, they told her she had 18 months. Now? She’s hiking in Colorado. Because someone finally looked at the DNA, not just the scan. That’s the power of precision. Don’t let fear silence your questions.
Kevin Lopez
January 2, 2026 AT 06:16Grade 4 = glioblastoma. IDH-wildtype = median 14.6mo. IDH-mutant = 31mo. MGMT methylated = temozolomide works. Non-methylated = useless. 1p/19q co-deletion = oligodendroglioma. No codeletion = not oligo. Vorasidenib = only for IDH-mutant grade 2. No exceptions. Stop guessing. Test. Then treat.
Teresa Rodriguez leon
January 2, 2026 AT 22:58I read this whole thing and cried. Not because I’m scared-but because I finally understand what my brother’s diagnosis really means. I didn’t know molecular testing could change everything. I thought ‘grade 2’ meant ‘it’s not cancer.’ It’s not just cancer. It’s a ticking clock with a DNA code. And now I know what to ask for.
Louis Paré
January 4, 2026 AT 03:51Another article glorifying American medical superiority. Meanwhile, in Canada, we wait six months for an MRI, then another three for a pathologist who can read a slide. Molecular testing? Only in Toronto. The rest of us get ‘probably benign’ and a pat on the head. Progress? Sure. For the privileged.
Janette Martens
January 5, 2026 AT 05:24So if u got a grade 2 tumor and its IDH mutated u get to live longer? Cool. But what if u dont got insurance? Or live in a state that dont cover testing? Then u just die slow? This system is broken. Science is great but people are still suffering.
Manan Pandya
January 7, 2026 AT 03:54As someone from India, I’ve seen firsthand how access to molecular diagnostics is a luxury. But I’ve also seen patients who, despite limited resources, insisted on testing because they refused to be treated blindly. Knowledge is power-but equity is justice. We need global standards, not just American breakthroughs.
Aliza Efraimov
January 9, 2026 AT 02:13When I was diagnosed with a grade 2 oligodendroglioma, I asked for the 1p/19q test. My neuro-oncologist said, ‘We don’t do that here.’ I drove three hours to a cancer center that did. That test changed everything. My treatment plan went from ‘watch and wait’ to ‘targeted therapy in 6 months.’ Don’t settle. Demand the data. Your life depends on it.
Nisha Marwaha
January 10, 2026 AT 16:43Let’s be real-most oncologists still think ‘histology’ is the gold standard. But the data doesn’t lie: two tumors that look identical under the microscope can have survival curves that diverge like highways. The 2021 WHO update isn’t academic-it’s a clinical imperative. If your center hasn’t trained their pathologists on IDH and 1p/19q, they’re operating in the 2010s.
Duncan Careless
January 12, 2026 AT 08:34Just read this after my sister’s diagnosis. Took me 3 days to understand half of it. But one thing stuck: ‘Don’t accept a grade without an IDH test.’ So I printed this out, took it to her appointment, and asked. They hadn’t done it. Now they’re sending it out. Small step. Huge difference.