If you’ve ever been told by your doctor that you need to try a cheaper drug before they can prescribe the one you really need, you’ve run into step therapy. It’s not a suggestion. It’s a rule. And it’s built into your insurance plan-whether you know it or not.
Step therapy, also called a "fail-first" policy, forces you to try one or more lower-cost medications-usually generics-before your insurer will pay for the drug your doctor originally prescribed. This isn’t about saving a few dollars on a prescription. It’s a system designed to cut overall drug spending, often at the cost of your time, comfort, and sometimes your health.
How Step Therapy Actually Works
Imagine you have rheumatoid arthritis. Your doctor recommends a biologic medication that works well for many patients. But your insurance doesn’t cover it right away. Instead, they require you to try three different generic anti-inflammatory drugs first. If those don’t work-or if they cause side effects-you can ask for an exception. But that process isn’t instant. It can take weeks.
This isn’t rare. About 40% of all prescription drug plans in the U.S. use step therapy, according to a 2021 analysis by the National Institutes of Health. Most employer-sponsored plans include it. So do many Medicare Part D and private insurance plans.
The structure is simple: Step 1 is usually a generic drug. Step 2 might be a brand-name drug that’s cheaper than the one your doctor wants. Step 3 is the drug you actually need. You have to fail at each step before moving up. And "fail" doesn’t just mean it didn’t work-it can mean you had a bad reaction, couldn’t tolerate it, or it just didn’t help enough.
Why Insurers Use Step Therapy
Drug prices in the U.S. are among the highest in the world. Insurers didn’t create these prices, but they’re the ones stuck paying them. So they use step therapy as a way to control costs.
According to a 2021 Congressional Budget Office report, step therapy can reduce pharmaceutical spending by 5% to 15% depending on the condition. For insurers, that’s a big win. For patients, it’s often a gamble.
Insurers argue they’re making sure patients get the most cost-effective treatment first. They say most people respond well to generics. And in some cases, they’re right. About 17% of patients surveyed by GoodRx in 2023 found their condition managed just fine with the required generic, avoiding the need for expensive drugs altogether.
But here’s the problem: not everyone responds the same way. For people with chronic conditions like multiple sclerosis, lupus, or severe psoriasis, waiting weeks or months to get the right drug can mean irreversible damage.
When Step Therapy Hurts More Than Helps
The American College of Rheumatology doesn’t support step therapy. Why? Because patients are getting worse while waiting.
A 2022 survey by the Arthritis Foundation found that 68% of patients experienced negative health outcomes because of step therapy. Over 40% reported disease progression during the required drug trials. One Reddit user, "ChronicPainWarrior," shared how they spent six months trying three different NSAIDs before getting approval for a biologic. By then, their joint damage had worsened significantly.
It’s not just arthritis. People with Crohn’s disease, depression, and even asthma have reported delays in treatment that led to hospitalizations, lost workdays, or permanent complications.
And it’s not just about effectiveness. Some medications can be dangerous if you’ve already tried others. For example, switching from one antidepressant to another without proper overlap can trigger severe withdrawal or worsen symptoms. But insurers don’t always account for that.
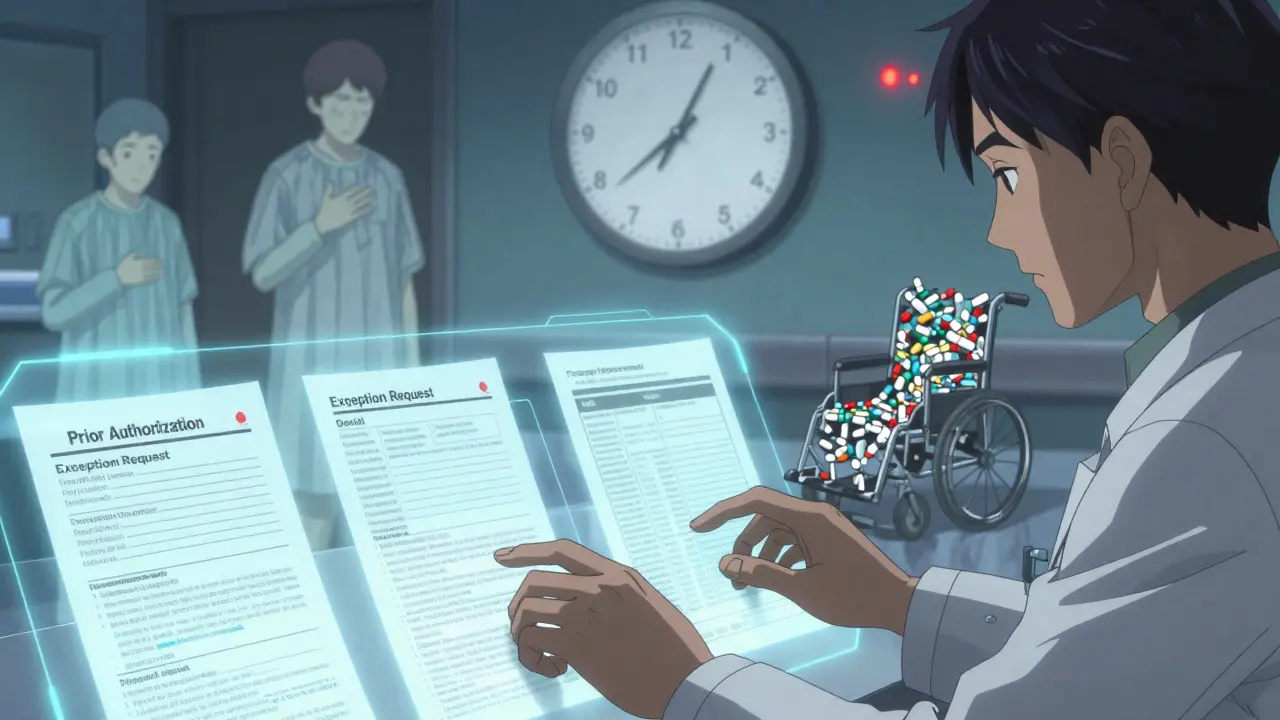
What You Can Do: Step Therapy Exceptions
You’re not stuck. Federal and state laws require insurers to allow exceptions.
Under the Safe Step Act (reintroduced in 2021), insurers must grant exceptions in five clear situations:
- You’ve already tried the required drug and it didn’t work
- The required drug would cause serious or irreversible harm
- The required drug is contraindicated with your other medications or health conditions
- Delaying treatment would prevent you from doing daily activities
- You’re already stable on the prescribed drug and have been covered for it before
But getting an exception isn’t easy. Your doctor has to submit medical records proving one of these conditions applies. That means paperwork, phone calls, and sometimes multiple appeals.
Blue Cross Blue Shield of Michigan says they review standard exceptions in 72 business hours. Urgent cases get a 24-hour turnaround. But that’s not universal. Some insurers take four to eight weeks. And if your doctor’s office is understaffed, they might not even start the process right away.
Doctors are drowning in paperwork. The American College of Rheumatology found that physicians spend an average of 18.3 hours per week just handling prior authorizations and step therapy requests. That’s nearly half a workday. Many don’t have the time or resources to push back.
State Laws vs. Self-Insured Plans
Here’s where it gets messy. Twenty-nine states have passed laws to protect patients from abusive step therapy rules. These laws require faster reviews, clearer exception criteria, and limits on how many steps you must go through.
But here’s the catch: those laws don’t apply to everyone. About 61% of Americans get their insurance through self-insured employer plans. These are run by large companies (like Walmart, Apple, or Google) that pay for their employees’ healthcare directly instead of buying insurance from a company like UnitedHealth or Aetna.
Self-insured plans are regulated by the federal government under ERISA, not state laws. So even if your state has strong protections, your employer’s plan can still force you through a five-step process with no time limits.
That’s why the Safe Step Act matters. It would require all self-insured plans to follow the same exception rules as fully-insured plans. But as of 2025, it hasn’t passed.

What You Should Do Right Now
If you’re on a medication that’s being blocked by step therapy:
- Ask your doctor if they’ve submitted an exception request. Many don’t do it automatically.
- Get a copy of your insurance plan’s step therapy policy. It’s usually on their website under "Drug Coverage" or "Prior Authorization Requirements."
- Check if your condition qualifies for an exception under the five federal criteria.
- If your doctor says no, ask them to document why the required drugs won’t work for you. Use specific terms: "contraindicated," "risk of irreversible damage," "previous failure."
- Call your insurer directly. Ask for the name of the person handling your case and follow up in writing.
Some patients have had success by contacting their employer’s HR department. If enough employees complain, companies can pressure their insurer to change the policy.
Alternatives to Step Therapy
If your insurer won’t budge, here are two real-world options:
- Pharmaceutical assistance programs: Nearly 80% of major drug makers offer co-pay cards or free medication programs for eligible patients. These can bypass step therapy entirely because the drug is being paid for by the manufacturer, not your insurer.
- Switch plans during open enrollment: If you’re choosing insurance next year, look at formularies. Some plans have fewer step therapy requirements. Use tools like Medicare’s Plan Finder or private comparison sites to see which plans cover your medication without forcing you to fail first.
And if you’re on a generic drug that works? Great. Step therapy did its job. But if you’re stuck on something that’s not working, you’re not being difficult. You’re being smart.
The Future of Step Therapy
Step therapy isn’t going away. Drug prices are still rising. Insurers need tools to manage costs. But the system is broken when it delays care for people with life-altering conditions.
Industry analysts at Avalere Health predict that by 2025, step therapy will apply to 55% of specialty drug prescriptions-up from 40% today. That means more people will face this hurdle.
The push now is for faster decisions, clearer rules, and better protections for vulnerable patients. Until then, you need to know your rights-and how to fight for them.
Step therapy isn’t about saving money. It’s about who pays the price.
What is step therapy in health insurance?
Step therapy is a rule used by health insurers that requires patients to try one or more lower-cost, usually generic, medications before the insurer will pay for a more expensive drug prescribed by their doctor. It’s also called a "fail-first" policy because you must prove the cheaper options didn’t work before moving up.
Why do insurers make me try generics first?
Insurers use step therapy to control rising drug costs. Generic drugs cost a fraction of brand-name drugs, so requiring them first reduces overall spending. While this saves money for the plan, it can delay effective treatment for patients who need a specific medication.
Can I skip step therapy if my doctor says I need a specific drug?
Yes, but you have to request an exception. Federal rules require insurers to grant exceptions if the required drug won’t work for you, could cause harm, or if you’re already stable on your current medication. Your doctor must submit medical records supporting your case.
How long does a step therapy exception take to get approved?
Standard requests usually take 72 business hours, but many insurers take four to eight weeks. Urgent cases-like those where delay could cause serious harm-should be reviewed in 24 hours. But in practice, delays are common, and many patients give up before getting a decision.
Are step therapy rules the same in every state?
No. Twenty-nine states have laws that protect patients by requiring faster reviews and clearer exception rules. But these laws don’t apply to self-insured employer plans, which cover about 61% of Americans. Those are regulated by federal law, and protections there are weaker.
What if I switch jobs and my new insurance requires me to start step therapy again?
That’s a common and dangerous problem. Even if you’ve been on the same medication for years, your new insurer can force you to restart the step therapy process. This can lead to treatment interruptions and worsening health. You should immediately request an exception based on prior stable use and provide documentation from your previous plan.
Can pharmaceutical companies help me bypass step therapy?
Yes. About 78% of major drug makers offer patient assistance programs, including co-pay cards or free medication for eligible patients. These programs pay for the drug directly, so your insurance doesn’t get involved. Ask your doctor or pharmacist if your medication has one.



James Rayner
December 16, 2025 AT 11:18It’s funny… we talk about "cost savings" like it’s a virtue, but what we’re really doing is trading human suffering for balance sheets. I’ve watched my sister go from mild joint pain to needing a wheelchair because they made her try five generics before letting her on the biologic. She didn’t "fail"-the system failed her. And now? She’s on disability. The insurer saved $3,000 a month. She lost her career. And nobody’s apologizing.
It’s not medicine. It’s a gamble with someone else’s body.
🫂
Kayleigh Campbell
December 17, 2025 AT 14:42So step therapy is just insurance’s way of saying "try this cheap junk first, and if you die, we’ll cover the funeral."
Classic.
Also, I’m pretty sure my doctor’s office has a shrine to the word "prior authorization" now. It’s just a pile of fax machines and despair.
💀
Joanna Ebizie
December 18, 2025 AT 08:54My cousin’s kid has juvenile arthritis. They made him take ibuprofen for 6 months. Six. Months. He ended up in the ER with a ruptured tendon because the "generic first" rule didn’t care that he couldn’t walk. Now the insurance pays for his surgery. Guess who’s paying the real cost?
Not them.
They’re just happy they didn’t have to shell out for the biologic upfront.
People are not data points.
Andrew Sychev
December 19, 2025 AT 12:05This is why I stopped trusting the entire medical-industrial complex. It’s not about your health-it’s about the bottom line. The same people who tell you to "take responsibility for your health" are the ones who’ll make you suffer for months just to save $200 a month on a drug. They don’t care if you’re in pain. They care if you’re profitable.
And don’t even get me started on how they bury the exception forms in 14-page PDFs no one reads.
This isn’t capitalism. It’s torture with a claims department.
Cassandra Collins
December 20, 2025 AT 19:15Okay but what if this is all just a secret ploy by Big Pharma to make you take the expensive drug later? Like… what if the generics are actually designed to fail? What if the companies that make the expensive drugs pay the insurers to make you suffer first so you’ll beg for their $10,000/month miracle drug? I’ve seen this in documentaries. They do this stuff. It’s not conspiracy-it’s corporate strategy.
They want you hooked. They want you dependent. And they want you to think you had no choice.
Wake up.
They’re playing you.
And your doctor? Probably getting kickbacks. Just saying.
Billy Poling
December 22, 2025 AT 18:46It is imperative to acknowledge that the utilization of step therapy protocols is not an inherently nefarious practice, but rather a clinically informed mechanism designed to optimize pharmacoeconomic outcomes. The assertion that such policies are uniformly detrimental to patient welfare is an oversimplification that disregards empirical data demonstrating that a significant proportion of patients achieve therapeutic efficacy with first-line generic agents. Moreover, the administrative burden placed upon providers, while substantial, is mitigated through standardized electronic prior authorization platforms that have been widely adopted by major payers. To characterize this as a systemic failure is to ignore the broader context of cost-containment measures that have enabled millions of patients to access otherwise unaffordable therapies. The ethical imperative lies not in abolishing step therapy, but in refining its implementation with greater clinical nuance and expedited exception pathways.
Souhardya Paul
December 24, 2025 AT 00:48I’ve been a pharmacist for 18 years, and I’ve seen this play out every day. The system isn’t broken-it’s just poorly designed. Most docs don’t even know how to file exceptions properly. And insurers? They don’t train their reps to help-they train them to delay.
Here’s what works: if you’re on a biologic, ask your pharmacist for the manufacturer’s patient assistance card. It’s not a secret. They give them out like candy. I’ve gotten people on $0 co-pays for $12k/month drugs because the pharma company doesn’t want them switching to a competitor.
Also-call your HR. If five people in your company complain, they’ll change the plan next year. I’ve seen it happen.
You’re not alone. You just need to be louder than the bureaucracy.
Elizabeth Bauman
December 25, 2025 AT 13:52Let’s be real-this is what happens when you let bureaucrats run healthcare. We used to have real medicine in this country. Now we’ve got robots in call centers reading scripts while your arthritis gets worse. And the worst part? The same people who run these plans are the ones who voted for the politicians who let this happen.
It’s not about money. It’s about control. They want you dependent. They want you silent. They want you too tired to fight.
But you know what? We’re not going to let them win. If you’re reading this and you’re stuck in step therapy-call your congressperson. Write your senator. Share your story. This isn’t just about drugs. It’s about dignity.
And if you think this is just a "healthcare issue," you’re not paying attention.
We’re being disarmed. Slowly. Quietly.
Don’t let them do it to you.
Ron Williams
December 27, 2025 AT 10:56Just want to say-I’m from a rural town in Nebraska. We don’t have rheumatologists. We have one GP who does his best. My mom had to wait 11 weeks for an exception because the insurance company lost the fax. She finally got her drug. Now she walks again.
But here’s the thing: she didn’t have a lawyer. Didn’t have a case manager. Just a phone and a prayer.
So if you’re reading this and you’re in a big city with resources? Help someone who doesn’t. Send them this post. Call their doctor’s office and ask if they need help filing. It takes five minutes.
That’s the real step therapy: helping each other climb.
Mike Smith
December 28, 2025 AT 20:41Step therapy is not the enemy-indifference is.
Every time a patient is told, "Just try it," and no one follows up, that’s the real failure.
Your doctor is overworked. Your insurer is profit-driven. But YOU are the only one who can advocate for your own body.
Don’t wait for permission. Don’t wait for a miracle. Document everything. Save every email. Call your insurer every 48 hours. Ask for a supervisor. Ask for the name of the person reviewing your case. Then call again and ask for them by name.
They hate that.
And that’s why it works.
You are not a claim number. You are not a cost center.
You are human.
And you deserve better.
Kitty Price
December 29, 2025 AT 03:55My mom’s rheumatoid arthritis got so bad she couldn’t hold a spoon. They made her try 4 generics. She cried every time she took them because they made her dizzy and nauseous. But she kept taking them because she didn’t want to be "that patient."
Then she found out she could get the real drug for free through the manufacturer’s program. She didn’t even need insurance.
She’s been pain-free for two years now.
Just… ask.
It’s not your fault if no one told you.
But now you know.
❤️
Aditya Kumar
December 31, 2025 AT 01:23eh idk man i just take what my doc says and dont think about it
Josias Ariel Mahlangu
December 31, 2025 AT 05:19People need to stop expecting the government or insurance companies to fix their problems. If you can’t afford your medication, you shouldn’t be taking it. There are cheaper alternatives. There are natural remedies. There’s discipline. You want a miracle drug? Work for it. Don’t expect someone else to pay for your weakness.
My grandfather had diabetes in the 1950s. He walked five miles to the clinic every week. He didn’t complain. He didn’t file appeals. He lived.
Maybe we need less entitlement and more grit.
Just saying.
Dylan Smith
January 1, 2026 AT 00:33Okay but what if the real problem is that drug companies charge $10k a month for pills that cost $2 to make? Why are we blaming insurers? They’re just trying to keep premiums from exploding. The real villains are the pharma CEOs who make $100M a year while patients go broke.
Step therapy is a symptom-not the disease.
And if you think the answer is to ban it, you’re not thinking big enough.
We need price caps. We need generic competition. We need to break the patent monopolies.
Until then? Yeah, step therapy sucks. But at least it’s not letting the drug companies bleed us dry without a fight.
Colleen Bigelow
January 2, 2026 AT 17:07Let’s not pretend this is about healthcare. This is about the deep state. The same people who run the insurance companies also run the FDA. They’re the same people who approved the vaccines, the same people who told you to wear masks, the same people who told you to get the shot. They’re not here to help you. They’re here to control you.
Step therapy? It’s just another way to track you. To monitor you. To make you dependent on their system.
And if you think your doctor is on your side? Think again. They’re paid by the same system. They’re just actors in the play.
Wake up.
Their goal isn’t your health.
It’s your compliance.
Billy Poling
January 3, 2026 AT 04:02While I appreciate the emotional narratives presented, I must reiterate that the data consistently demonstrate that step therapy reduces overall pharmaceutical expenditures without significantly compromising clinical outcomes in the majority of cases. The anecdotal exceptions, though deeply unfortunate, do not invalidate the broader public health benefit of cost-containment strategies. Moreover, the assertion that insurers are deliberately delaying care is not substantiated by audit data from CMS, which shows that over 87% of exceptions are resolved within 72 hours when properly documented. The real issue lies not in policy design, but in inconsistent implementation by providers who fail to submit adequate clinical justification. The solution is not abolition, but standardization and provider education.