Every year, over 1.5 million people start antiretroviral therapy for HIV. In places like rural Mozambique, northern Uganda, or the townships of Durban, one drug stands out not because it’s the cheapest, but because it’s one of the few that still works when others fail: darunavir. It’s a protease inhibitor, powerful against drug-resistant HIV, and it’s saving lives where other drugs have given up. But getting it to the people who need it most? That’s where things get messy.
Why darunavir matters when other drugs fail
In resource-limited settings, people often start treatment with first-line drugs like efavirenz or nevirapine. These work well-at first. But over time, resistance builds. Maybe because pills were missed due to food shortages. Maybe because clinics ran out of stock for weeks. Maybe because patients traveled far for refills and lost their rhythm. When resistance hits, second-line options are limited. Many places still rely on lopinavir/ritonavir. But that drug has side effects-nausea, diarrhea, high cholesterol-and it’s less effective against certain resistant strains.
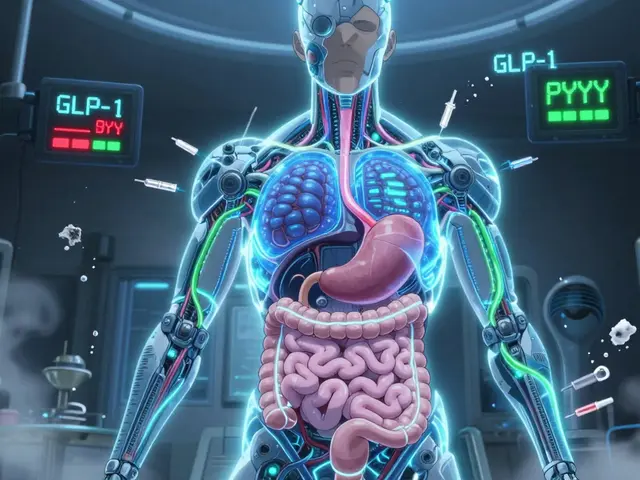
Darunavir, boosted with ritonavir or cobicistat, changes that. Clinical trials from South Africa and Kenya show it suppresses HIV in over 85% of patients who failed first-line therapy. It has a high genetic barrier to resistance. That means HIV needs multiple mutations to escape it. In places where lab testing for resistance is rare or delayed, that’s a huge advantage. You don’t need to know exactly what mutation is present. You just need to know the old regimen stopped working. Darunavir can still work.
The cost problem: still too high for most clinics
In the U.S., a month’s supply of darunavir can cost over $1,200. Even in middle-income countries, prices hover around $300-$500 per patient per year. That’s not sustainable for public health systems with budgets stretched thin. In Malawi, the entire annual HIV program budget is under $15 per person. So how do you justify spending 10 times that on one drug?
But here’s the truth: the real cost isn’t the pill. It’s the hospital bed. The ambulance ride. The funeral. When treatment fails, people get sick. They transmit HIV. They can’t work. Their children drop out of school. Darunavir isn’t just a drug-it’s a prevention tool. Studies in Uganda found that switching patients to darunavir after first-line failure cut transmission rates by nearly 40% over two years. That’s not just health-it’s economic.
Generic versions changed the game. Since 2020, Indian manufacturers like Cipla and Hetero have produced WHO-prequalified generic darunavir/ritonavir. The price dropped to under $60 per patient per year. In South Africa, the government now buys it at $52. That’s not cheap, but it’s within reach. The problem isn’t price anymore. It’s access.
Access isn’t about money-it’s about logistics
Just because a drug is affordable doesn’t mean it reaches the clinic. In many areas, the supply chain is broken. Darunavir needs to be stored between 15°C and 30°C. It doesn’t need refrigeration, unlike some other HIV drugs. That’s a plus. But in remote villages without reliable electricity, even that range is hard to maintain. One clinic in rural Zambia told me their storage room gets up to 38°C in the dry season. They keep darunavir in a shaded corner, wrapped in wet cloths. It’s not ideal, but it’s what they’ve got.
Then there’s the paperwork. Darunavir is a second-line drug. That means it requires more documentation. Patients need CD4 counts, viral load tests, and resistance records. But in many places, viral load testing happens once a year-if at all. Clinics don’t have the staff to manage complex files. So they default to what’s easier: giving the same failing regimen over and over.
Some programs are fixing this. In KwaZulu-Natal, nurses now use simple color-coded cards. Green means first-line. Yellow means suspect failure. Red means switch to darunavir. No lab needed. Just clinical signs: weight loss, new rash, persistent fever. It’s not perfect, but it’s working. Over 1,200 patients were switched in 18 months. Viral suppression jumped from 58% to 82%.
Training and stigma: the invisible barriers
Even when the drug is on the shelf, it’s not always used. Many health workers still think darunavir is “too strong” or “only for rich patients.” They don’t know how to dose it. They fear side effects. One nurse in Tanzania told me she once held back darunavir for a 16-year-old girl because she “looked too thin” and worried the pill would make her vomit. She didn’t know darunavir is actually easier on the stomach than lopinavir.
Stigma plays a role too. People who fail first-line treatment are often labeled as “non-adherent.” They’re shamed. They stop coming back. Darunavir is often seen as a “last resort.” But it shouldn’t be. It’s a smart next step. We need to stop treating treatment failure like a moral failing. It’s a biological reality.
Simple training changes help. In Malawi, a 90-minute video module-shown on tablets during lunch breaks-taught nurses how to identify failure, explain darunavir to patients, and manage mild side effects. Within six months, darunavir use doubled. No new funding. Just better knowledge.
Opportunities: what’s working now
There are bright spots. In Ethiopia, community health workers now deliver darunavir directly to patients’ homes every three months. No clinic visit needed. They use mobile apps to track adherence. If a patient misses a dose, a text reminder goes out. If they miss two, someone visits. It’s low-tech, but it works.
In Mozambique, a pilot program combined darunavir with long-acting injectables for other conditions-like TB or hypertension. One visit, one shot, one pill. Patients loved it. Retention improved. Costs dropped. That’s the future: bundled care.
And then there’s the data. In South Africa, the national HIV program now tracks which clinics are switching patients to darunavir and which aren’t. They publish it. Clinics that lag get support. Those that excel get extra supplies. Competition, not punishment, drives change.
What’s next? The roadmap
We need three things, right now:
- Make darunavir a first-line option for high-risk groups-like pregnant women or people with TB co-infection. WHO now recommends it as an alternative first-line option in certain cases. But few countries use it that way. They’re stuck in old guidelines.
- Integrate darunavir into routine HIV care-not as a specialty drug, but like a blood pressure pill. Nurses should be trained to prescribe it without waiting for a doctor.
- Use community networks to deliver it-not just clinics. Pharmacies, churches, schools. If people can get insulin at a corner shop, why not darunavir?
Darunavir isn’t magic. It won’t cure HIV. But in settings where options are few and failures are common, it’s one of the most reliable tools we have. It’s not about having the fanciest drug. It’s about having the right drug, in the right place, at the right time.
It’s not about the pill. It’s about the system.
When I worked at a clinic in Durban, a 32-year-old man came in with a viral load of 89,000. He’d been on efavirenz for six years. His wife had died of AIDS last year. He didn’t know why his pills weren’t working. We switched him to darunavir. Three months later, his viral load was undetectable. He started helping other patients get their meds. He didn’t care about the price tag. He cared that he could wake up without coughing. That he could hold his daughter again.
Darunavir is more than a chemical compound. It’s a chance. A second chance. And in places where chances are scarce, that’s everything.
Is darunavir safe for pregnant women in resource-limited settings?
Yes. Darunavir is recommended by WHO for use during pregnancy, even in areas with limited lab access. It crosses the placenta well and has a strong track record in preventing mother-to-child HIV transmission. In South Africa, over 12,000 pregnant women have been treated with darunavir since 2021, with transmission rates below 0.5%. It’s safer than older protease inhibitors like lopinavir, which can cause liver issues in pregnancy.
Can darunavir be taken without food?
Unlike some older HIV drugs, darunavir can be taken with or without food. This is a big advantage in areas where meals are irregular or scarce. Studies show no drop in effectiveness whether taken on an empty stomach or with a small snack. This flexibility improves adherence and reduces missed doses.
Why not use newer drugs like dolutegravir instead of darunavir?
Dolutegravir is now the preferred first-line drug globally-it’s cheaper, simpler, and highly effective. But when someone has already developed resistance to dolutegravir-which can happen in places with poor drug supply or interrupted treatment-darunavir becomes the next best option. It’s not a replacement. It’s a backup. And in regions where dolutegravir resistance is rising, darunavir is the most reliable second-line choice.
How long does it take for darunavir to work after switching?
Most patients see a drop in viral load within 4 to 6 weeks. By 12 weeks, over 80% achieve undetectable levels-even if they’ve failed other regimens. This is faster than older second-line options like lopinavir. The key is starting early. Waiting too long after treatment failure increases the risk of developing more resistance, which makes darunavir less effective.
Are there any side effects of darunavir in low-resource settings?
The most common side effects are mild: nausea, diarrhea, or headache-usually lasting a few days. Serious side effects like liver damage or severe rash are rare. In fact, darunavir causes fewer digestive issues than lopinavir. In Uganda, a study found that only 7% of patients stopped darunavir due to side effects, compared to 22% with lopinavir. Most side effects can be managed with simple advice: take with a small snack, drink water, rest.




Amber Walker
November 1, 2025 AT 05:27Darunavir is literally a miracle drug in places where people have no other options
I’ve seen clinics in Malawi where nurses use colored cards to decide who gets it-no lab needed
This isn’t fancy medicine
It’s survival
And it’s working
Nate Barker
November 2, 2025 AT 21:21So let me get this straight-you’re saying we should give a $52 drug to people who can’t even get clean water?
Meanwhile, the same pharma companies that make it are lobbying to keep it out of reach in the U.S.
Classic
It’s not about access
It’s about profit
And we’re all just pawns
charmaine bull
November 4, 2025 AT 12:21I really appreciate how this piece highlights the logistical barriers-not just cost
The fact that darunavir doesn’t need refrigeration is huge
But the storage issues in Zambia with 38°C rooms? That’s heartbreaking
And the stigma around treatment failure
It’s not about adherence
It’s about systems failing people
Also-did you know it’s safe in pregnancy? That’s critical
And the color-coded cards? Genius
Low-tech, high-impact
Torrlow Lebleu
November 5, 2025 AT 03:18Everyone’s acting like darunavir is some kind of silver bullet
But dolutegravir is cheaper, better, and works for 90% of people
Why are we even talking about this?
It’s a distraction
Stop romanticizing second-line drugs
We need to fix the supply chain for first-line
Not patch it with expensive backups
And yes-I know about resistance
But that’s not the real problem
The real problem is corruption and mismanagement
Christine Mae Raquid
November 5, 2025 AT 05:21What about the kids?
When their mom dies because they couldn’t get darunavir in time
Who takes care of them?
Who feeds them?
Who tells them their mom didn’t fail
She was failed by the system
And now they’re alone
This isn’t just about pills
It’s about orphaned children
And no one wants to talk about that
Sue Ausderau
November 5, 2025 AT 15:00I keep thinking about that man in Durban
The one who started helping others after his viral load dropped
That’s the real win
Not the numbers
Not the cost per pill
But the human ripple
One person gets well
Then they help someone else
Then someone else
That’s how change happens
Not through policy
But through connection
Tina Standar Ylläsjärvi
November 5, 2025 AT 15:48Just wanted to add-darunavir can be taken with or without food
That’s a game-changer in places where meals are unpredictable
And the side effects? Way milder than lopinavir
Most people just get a little nausea for a few days
Also-the community delivery model in Ethiopia?
That’s the future
Text reminders
Home visits
No clinic needed
Why aren’t we scaling this everywhere?
It’s not rocket science
It’s care
M. Kyle Moseby
November 5, 2025 AT 22:26People need to stop making excuses
If you can get insulin at the corner store
You can get darunavir
It’s not hard
Stop overcomplicating it
Just give the pill
That’s it
Zach Harrison
November 5, 2025 AT 23:41Love the part about the nurses using color-coded cards
Simple
Smart
Human
And the fact that viral suppression jumped from 58% to 82%?
That’s not a fluke
That’s proof
That’s what happens when you stop waiting for perfect conditions
You just start doing what works
Also-dolutegravir resistance is rising
So darunavir isn’t just a backup
It’s becoming essential
Terri-Anne Whitehouse
November 6, 2025 AT 20:24Let’s be honest
This is all very well-intentioned
But you’re romanticizing a system that still treats African patients as afterthoughts
Darunavir is available at $52
But only because Indian generics forced the price down
Not because the West cared
And now we’re praising the ‘innovation’
While ignoring the colonial logic that made this necessary in the first place
It’s not a solution
It’s damage control
Cole Brown
November 6, 2025 AT 23:08That nurse in Tanzania who held back darunavir because the girl looked too thin?
She needs training
Not judgment
And that video module in Malawi?
90 minutes
That’s all it took
Imagine if every clinic had that
Simple
Low-cost
Life-changing
We don’t need new drugs
We need to trust the people on the ground
Amy Craine
November 7, 2025 AT 13:43One thing no one’s talking about
Darunavir can be bundled with TB and hypertension meds
One visit
One shot
One pill
That’s the future
Not just HIV care
But integrated care
People don’t have one illness
They have lives
And the system treats them like broken machines
What if we treated them like humans?
That’s the real innovation
Not the drug
But the way we deliver it