Medication Risk Assessment Tool
Your Risk Profile
Medication Check
Risk Assessment Results
Imagine waking up with a throbbing headache, blurry vision, and halos around lights. You feel nauseous. Your eye feels like it’s swelling shut. You go to the ER, and they give you a migraine pill. But it’s not a migraine. It’s acute angle-closure glaucoma-and it’s being triggered by something you took for a cold, allergies, or even anxiety. This isn’t rare. It’s preventable. And every year, hundreds of people lose part of their vision because no one checked if their eyes were at risk.
What Exactly Is Medication-Induced Acute Angle-Closure Glaucoma?
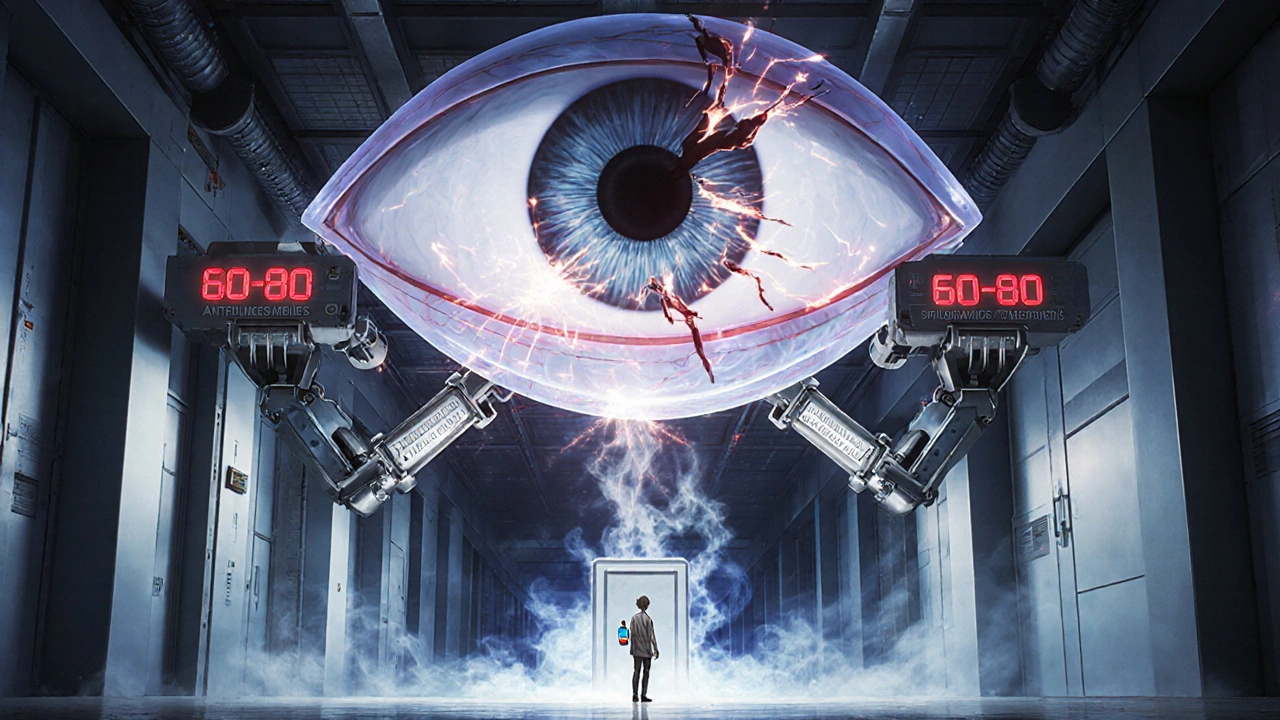
Acute angle-closure glaucoma (AACG) happens when the drainage angle inside your eye suddenly closes. This angle is where fluid normally drains out of your eye. When it blocks, pressure spikes-fast. In a healthy eye, pressure stays between 10 and 21 mm Hg. In AACG, it can jump to 60, 70, even 80 mm Hg. That’s like putting your eye under water pressure at 20 feet deep. And if it stays that high for more than 24 hours, you risk permanent blindness.
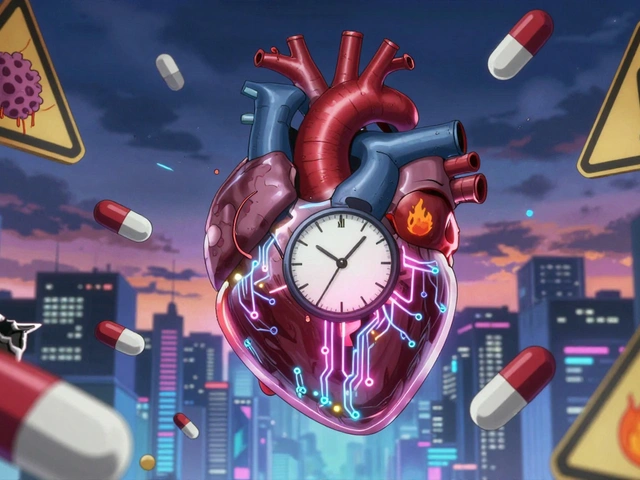
Most glaucoma creeps up slowly-like open-angle glaucoma. But AACG hits like a lightning strike. And when it’s caused by a medication, it’s called drug-induced AACG. It doesn’t happen to everyone. It happens to people with a hidden anatomical flaw: narrow drainage angles. These angles are too tight, like a door that’s almost shut. A single pill or eye drop can push the iris forward and slam it shut.
It’s not just about old age. Even young, healthy people can be at risk. The problem? Most people don’t know they have narrow angles until it’s too late. Only about 25% of those who end up with drug-induced AACG had ever been told they were at risk.
Which Medications Can Trigger This Emergency?
You might be surprised. These aren’t obscure drugs. They’re common, over-the-counter, and often prescribed without a second thought.
- Anticholinergics - Like tropicamide (used in eye exams), diphenhydramine (Benadryl), and oxybutynin (for overactive bladder). These drugs cause your pupil to dilate. In a narrow-angle eye, that’s like pulling a door shut with a string.
- Adrenergic agents - Phenylephrine (in nasal sprays and eye drops), ephedrine (in asthma inhalers), and pseudoephedrine (Sudafed). These stimulate the iris muscles and can physically block the drainage angle.
- Sulfonamide-based drugs - Acetazolamide (Diamox), sulfamethoxazole (Bactrim), and topiramate (Topamax for seizures or migraines). These can cause the ciliary body to swell, pushing the iris forward.
- SSRIs and tricyclic antidepressants - Paroxetine (Paxil), amitriptyline, sertraline. Even though they’re not anticholinergics, they have indirect effects on pupil control and can trigger angle closure.
- Antihistamines and decongestants - Found in cold and allergy meds. Many contain diphenhydramine or pseudoephedrine, both high-risk.
One study found that phenylephrine eye drops caused 35% of all medication-induced AACG cases. Tropicamide, the standard dilating drop used in routine eye exams, caused 28%. That means a simple eye check could turn into a vision disaster-if the doctor doesn’t check your angles first.
Who’s Most at Risk?
It’s not random. Certain people are built with a higher risk:
- Asian descent - People of East Asian heritage have an 8.5% chance of having narrow angles, compared to 3.8% in White populations. That’s more than double the risk.
- Farsightedness (hyperopia) - If you’re farsighted, your eyeball is shorter. That means the iris is crowded, and the angle is naturally tighter.
- Age over 40 - The lens thickens with age, pushing the iris forward and narrowing the angle further.
- Family history - If a close relative had AACG, your odds go up.
- Previous eye surgery or trauma - Even minor changes can alter the angle structure.
Ultrasound biomicroscopy and optical coherence tomography (OCT) can measure your anterior chamber depth. If it’s less than 2.5 mm, you’re in the danger zone. But most people never get this test unless they’re having cataract surgery.
What Are the Symptoms? Don’t Wait.
If you feel any of these, go to an emergency eye clinic immediately-not your primary care doctor, not the ER unless they have an ophthalmologist on call:
- Sudden, severe eye pain
- Blurred or foggy vision
- Seeing rainbow-colored halos around lights
- Red eye
- Headache, nausea, vomiting
- Fixed, mid-dilated pupil (doesn’t react to light)
These symptoms can come on in minutes. They’re often mistaken for migraines, sinus infections, or even food poisoning. A 2021 study of over 4,300 emergency room visits found that doctors correctly diagnosed AACG in only 38% of cases on the first visit. The average delay before correct diagnosis? 17 hours. That’s enough time to lose permanent vision.
How Is It Treated? Speed Is Everything
There’s no time for waiting. Treatment starts the moment AACG is suspected:
- Lower eye pressure fast - Pilocarpine eye drops (2%) every 15 minutes for an hour to pull the iris back. Oral or IV acetazolamide to reduce fluid production. IV mannitol to draw fluid out of the eye.
- Stop the triggering drug immediately - If you took Benadryl or Sudafed, stop it. If you had dilating drops, tell the doctor.
- Emergency laser procedure - Within 24 hours, a laser iridotomy is done. A tiny hole is burned in the iris to let fluid bypass the blocked angle. This is lifesaving for your vision.
- Long-term monitoring - Even after treatment, you’ll need regular check-ups. Your other eye is likely at risk too.
Without treatment, optic nerve damage begins within 6 hours. After 24 hours of pressure above 40 mm Hg, permanent vision loss is almost certain. This isn’t a "wait and see" situation. It’s a race against time.
How to Prevent It
The good news? This emergency is almost always preventable.
Before taking any new medication-especially if you’re over 40 or farsighted-ask your doctor:
- "Could this cause angle-closure glaucoma?"
- "Have you checked my drainage angles?"
- "Is there a safer alternative?"
If you’ve never had a gonioscopy (a simple 5-minute test where the doctor looks at your drainage angle with a special lens), get one-especially if you’re planning to take any of the high-risk drugs listed above. It’s quick, painless, and could save your sight.
For allergies, swap diphenhydramine for loratadine (Claritin). For nasal congestion, use saline sprays instead of phenylephrine. For overactive bladder, ask about mirabegron instead of oxybutynin. For migraines, avoid topiramate if you have narrow angles.
Some clinics now use electronic health records that flag high-risk prescriptions. Epic Systems, for example, now shows alerts when a doctor tries to prescribe a drug like acetazolamide to someone with a history of narrow angles. But not all systems do this. You have to be your own advocate.
What Patients Are Saying
On patient forums, the stories are heartbreaking:
- "Took Benadryl for allergies. Woke up blind in one eye. Took 36 hours to get diagnosed. Lost 20% of my peripheral vision. No one warned me." - VisionWarrior42, Glaucoma Forum
- "My eye doctor used tropicamide drops. I didn’t know I had narrow angles. Pressure shot to 60 mm Hg. Permanent damage. I’m 32." - OptomPatient2023, Reddit
A 2022 survey of 1,247 glaucoma patients found that 78% were never told about eye risks when prescribed high-risk medications. That’s not negligence-it’s systemic failure. Doctors aren’t always trained to think about eyes when prescribing pills. But you can change that.
What’s Being Done? And What’s Still Missing
Regulators are catching on. The FDA now requires black box warnings on drugs like topiramate and sulfonamides. The American Academy of Ophthalmology updated its guidelines in 2022 to say: "Do not use anticholinergics in patients with narrow angles unless absolutely necessary and under direct supervision."
But here’s the gap: Only 42% of primary care doctors routinely screen for glaucoma risk before prescribing these drugs. And 68% of patients say they received no counseling about eye risks at all.
Advanced tools like OCT can detect narrow angles with 94% accuracy. Genetic testing is emerging-17 genes linked to narrow angles have been identified. But these tools aren’t routine. They’re still mostly used in eye clinics, not in pharmacies or GP offices.
The solution? Make angle screening standard for anyone over 40 before prescribing high-risk drugs. Make it part of the prescription workflow. And educate patients: "This pill can blind you if you have narrow angles. Ask your eye doctor."
Can over-the-counter cold medicine cause acute angle-closure glaucoma?
Yes. Medications containing pseudoephedrine (like Sudafed) or diphenhydramine (like Benadryl) are common triggers. These drugs can cause pupil dilation or iris swelling, which blocks fluid drainage in eyes with narrow angles. Even a single dose can trigger an emergency in at-risk individuals.
How do I know if I have narrow angles?
You won’t know unless you get a gonioscopy-a quick, painless eye exam where an ophthalmologist uses a special lens to view your drainage angle. It takes about 5 minutes per eye. If you’re over 40, farsighted, or of East Asian descent, ask for this test before starting any new medication.
Is acute angle-closure glaucoma reversible?
If treated within 24 hours, vision can often be preserved. But if eye pressure stays above 40 mm Hg for more than a day, permanent optic nerve damage occurs. The earlier the treatment, the better the outcome. Delaying care-even by hours-can mean losing peripheral vision for life.
Can I still have eye exams if I have narrow angles?
Yes, but not with standard dilating drops like tropicamide. Your eye doctor can use alternative methods like OCT imaging or dilate your eyes under close monitoring with lower-risk agents. Always tell your eye care provider you have narrow angles before any exam.
Are there alternatives to high-risk medications?
Yes. For allergies, use loratadine (Claritin) instead of diphenhydramine. For nasal congestion, try saline sprays or oxymetazoline (short-term only). For overactive bladder, mirabegron is safer than oxybutynin. For migraines, avoid topiramate if you have narrow angles. Always ask your doctor for alternatives.
What to Do Next
If you’re over 40, farsighted, or have a family history of glaucoma: schedule a gonioscopy. Don’t wait for symptoms. If you’re about to start a new medication-especially for allergies, depression, bladder issues, or migraines-ask your doctor: "Could this affect my eyes?" Keep a list of high-risk drugs handy. Share it with your pharmacist.
If you’ve ever had sudden eye pain, blurred vision, or halos after taking a new pill-tell your eye doctor. Even if it happened months ago. That episode might have been a warning sign.
This isn’t about fear. It’s about awareness. Medication-induced AACG is one of the most preventable causes of sudden blindness. You don’t need a specialist to save your vision. You just need to ask the right question before you swallow that pill.




Arrieta Larsen
October 31, 2025 AT 12:46I took Benadryl last winter for a cold and woke up with a headache so bad I thought I was having a stroke. Turns out my eye pressure was 68. No one ever told me I had narrow angles. I’m 38, farsighted, and Asian. If this post saves one person’s vision, it’s worth it.
Mike Gordon
November 1, 2025 AT 08:26So… let me get this straight. A simple eye exam can prevent blindness? And doctors don’t do it? And we’re supposed to just… ask? Like, casually? "Hey doc, can you check if my eyeballs are shaped like a trapdoor?" No wonder people lose vision. It’s not the meds-it’s the system.
Prakash pawar
November 1, 2025 AT 13:42Bro this is why India has better eye care than the US. We know the body is a temple. You take a pill without knowing your anatomy? That’s not ignorance-it’s spiritual laziness. The West thinks medicine is a vending machine. But your eyes? They’re not a soda can. You don’t just pop a pill and pray. You must know your own structure. Otherwise you’re just a walking time bomb.
MOLLY SURNO
November 2, 2025 AT 03:32This is one of the most important posts I’ve read in years. I work in primary care and I’ve seen this happen twice. The delay in diagnosis is criminal. We need mandatory screening protocols. Not optional. Mandatory. And patients deserve better than being handed a script with zero warning.
Alex Hundert
November 3, 2025 AT 12:08Stop waiting for the system to fix this. If you’re over 40 or farsighted, go to an optometrist RIGHT NOW and ask for gonioscopy. It’s $50. It takes 10 minutes. If they refuse, go somewhere else. Your vision isn’t negotiable. I did this last year. My angles were 2.1 mm. I’m now on a no-diphenhydramine list. And I’m not apologizing for it.
Emily Kidd
November 3, 2025 AT 16:49just wanted to say i had this happen to me after taking sudafed. i thought it was a sinus infection. ended up in the er with my eye bulging out. they did the laser thing and saved my vision. but i had no idea i was at risk. now i tell everyone. if you take meds for allergies or anxiety, ask your eye doc. seriously. it’s that simple.
Justin Cheah
November 4, 2025 AT 18:46Here’s the real conspiracy: Big Pharma knows this happens. They don’t warn you because they’d lose billions if people stopped taking Benadryl, Sudafed, and Topamax. The FDA warning? A joke. It’s buried in the 200-page insert no one reads. They profit off blindness. And the medical system? It’s designed to treat symptoms, not prevent them. You think this is about health? No. It’s about profit. And you’re the product.
caiden gilbert
November 4, 2025 AT 19:52My cousin’s eye doctor called it "the silent trap"-like a bear trap for your vision. You walk in for a cold, get a pill, and boom. Your eye becomes a pressure cooker. And the worst part? You don’t feel it until it’s too late. It’s not pain you feel first-it’s the *absence* of clarity. Like your world got fogged with static. I’ve never seen someone so calm until their vision started crumbling. Now I carry a little card in my wallet: "No diphenhydramine. Narrow angles. Ask me."
phenter mine
November 6, 2025 AT 17:50im so glad i found this. i just started taking oxybutynin for my bladder and i didnt even think about my eyes. i’m farsighted and 47. i called my dr today and asked for a gonioscopy. they said "oh yeah we should’ve done that already." so i’m going next week. thanks for the heads up.
Aditya Singh
November 7, 2025 AT 00:46Let’s be clear: this is not a medical issue-it’s a failure of epistemology. The Western biomedical model reduces the eye to a hydraulic system while ignoring the phenomenological reality of perception. You cannot quantify anatomical risk without first acknowledging the ontological vulnerability of the human body. The fact that you need a 5-minute test to prevent irreversible damage speaks to the epistemic poverty of contemporary pharmacology.
Katherine Reinarz
November 7, 2025 AT 02:53OMG I JUST REALIZED I TOOK BENADRYL LAST WEEK AND I’M FARSIGHTED AND MY MOM HAD GLAUCOMA. I’M GOING TO THE ER RIGHT NOW. I FEEL A LITTLE BLURRY. IS IT HAPPENING? IS IT HAPPENING? I NEED TO KNOW NOW. I CAN’T SEE MY PHONE. I’M SCARED. SOMEONE TELL ME IF I’M GOING BLIND. I’M CRYING. I NEED HELP.
John Kane
November 8, 2025 AT 00:25Hey everyone, I just want to say how proud I am of all of you for sharing your stories. This is exactly what community is for-raising awareness, protecting each other, and turning fear into action. I’ve been an optometrist for 22 years and I’ve seen too many people lose vision because no one asked the right question. You’re doing the work. You’re being your own advocate. And that’s powerful. Don’t stop. Share this post. Talk to your parents. Text your siblings. Print out that list of high-risk meds and stick it on your fridge. One conversation could save a lifetime of sight.
Callum Breden
November 9, 2025 AT 01:42While the sentiment is laudable, the underlying premise remains fundamentally flawed. The notion that a 5-minute gonioscopy should be universally mandated prior to prescribing anticholinergics is not only logistically untenable but epistemologically unsound. The prevalence of narrow angles in the general population is insufficient to justify population-wide screening. The marginal benefit does not offset the cost, the resource allocation, nor the potential for iatrogenic anxiety. One must exercise prudence-not panic-in medical intervention. This post, while emotionally compelling, is a textbook example of alarmist medicalization.