When your production line stops because a temperature sensor reads 2.3°C off, or a torque wrench over-tightens screws by 15%, you’re not dealing with a random glitch. You’re facing the direct result of poor equipment calibration and unvalidated processes. In manufacturing-especially medical device production-this isn’t just a cost issue. It’s a patient safety issue.
Why Calibration Isn’t Just a Checklist
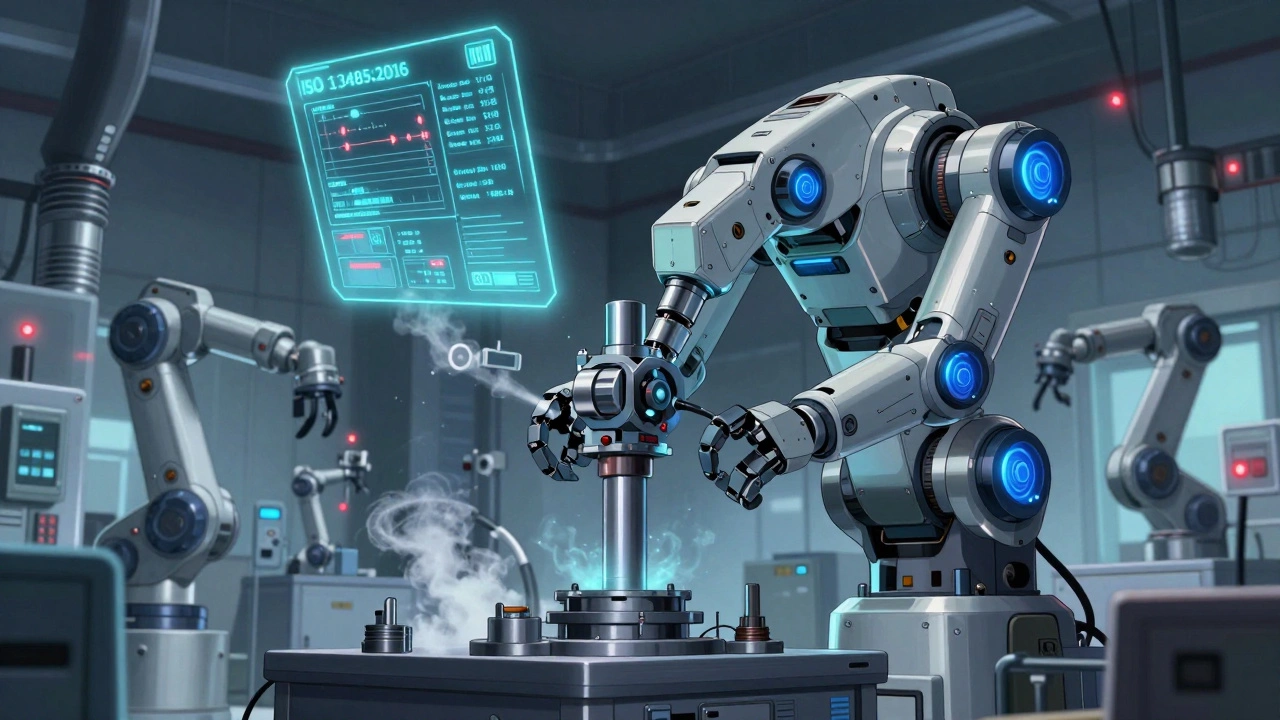
Calibration isn’t about making sure a device looks clean or runs quietly. It’s about proving, with documented evidence, that your measuring tool gives you the right number every time. ISO/IEC 17000 defines it clearly: calibration links what your instrument shows to a known standard-like a NIST-traceable weight or a calibrated thermometer. That chain must be unbroken, traceable to the International System of Units (SI), and include documented uncertainty values.Most manufacturers think calibration is just a yearly event. But ISO 13485:2016 says it must happen at specified intervals or prior to use. That means if you’re using a micrometer to measure a critical implant component after a weekend shutdown, you can’t just grab it off the shelf. You need proof it was checked and within tolerance before you started.
And here’s the kicker: 37.2% of FDA warning letters between 2020 and 2023 cited inadequate calibration. That’s not a small number. It’s the third most common compliance failure in medical device manufacturing. Companies aren’t failing because they don’t have tools-they’re failing because they don’t have a system.
What ISO 13485:2016 Actually Demands
ISO 13485:2016, Clause 7.6, doesn’t leave room for guesswork. Here’s what it requires:- Equipment must have a unique ID-no more "the red gauge in the corner".
- Calibration must be traceable to SI units through a documented chain of standards.
- Measurement uncertainty must be less than 25% of the tolerance you’re checking.
- Environmental conditions during calibration must be recorded-usually 20°C ±2°C and 40% RH ±10%.
- Records must be kept for at least the product’s lifecycle plus two years.
Let’s say you’re calibrating a digital scale used to weigh active pharmaceutical ingredients. The tolerance is ±0.05 grams. Your calibration standard must have an uncertainty of less than ±0.0125 grams. If your lab’s standard has ±0.015 grams, you’re already out of compliance-even if the scale reads perfectly.
And don’t assume your vendor’s calibration certificate is enough. If they don’t show the full traceability chain-down to the NIST or BIPM reference-you’re not compliant. Many small manufacturers get caught here. They pay for a certificate, file it away, and assume they’re covered. They’re not.
Calibration Intervals: One Size Does Not Fit All
The biggest mistake companies make? Using the same interval for everything.ISO 9001:2015 lets you set intervals based on risk and historical data. ISO 13485:2016 doesn’t forbid that-but it demands you prove it. That means you need data. Not opinions. Data.
Here’s how it works in practice:
- A high-precision micrometer in aerospace manufacturing? Calibrated every 3 months. It’s used daily, handles tight tolerances, and any drift could mean a rejected part.
- A basic thermometer in a food processing plant? Once a year. It’s stable, rarely moved, and the tolerance is ±2°C.
- A pH meter in a lab with 80% humidity? Monthly. Moisture causes drift. The manufacturer says 6 months? Irrelevant if your environment breaks it.
One biomedical engineer in Durban extended her lab’s electronic scale calibration from quarterly to biannually after collecting 18 months of stability data. Saved $18,500 a year. No audit findings. Why? Because she didn’t just follow a calendar-she used evidence.
Conversely, a lab in Cape Town kept their pH meters on a 6-month schedule despite humidity spikes. Their readings drifted by 0.4 units. Product batches failed. They lost $220,000 in recalls. The manufacturer’s recommendation didn’t matter. Their environment did.
Validation: When Calibration Isn’t Enough
Calibration tells you if your tool reads correctly. Validation tells you if your whole process works as intended.Think of it this way: You can calibrate a syringe filler to dispense exactly 5 mL. But if the tubing kinks every 30 cycles, or the valve sticks when the room hits 28°C, the machine still fails. That’s where validation comes in.
Validation follows GAMP 5 guidelines: three phases.
- Installation Qualification (IQ): Did you install the equipment right? Are the right parts there? Are environmental controls in place?
- Operational Qualification (OQ): Does it work under all expected conditions? Test extremes-low/high temperature, max/min speed, power fluctuations.
- Performance Qualification (PQ): Does it consistently produce acceptable results with real product? Run 10-30 batches. Document everything.
Medical device companies spend $25,000 to $500,000 validating a single production line. Why? Because a failed validation means your product can’t be sold. FDA won’t approve it. Insurance won’t cover it. Patients won’t trust it.
And software? Under FDA 21 CFR Part 11, even off-the-shelf software used in quality control needs validation. Not just the license key. You have to prove the algorithm doesn’t corrupt data. A 2024 case showed a company using a commercial LIMS system that auto-generated calibration reports. The software had a bug that flipped decimal points. They didn’t validate it. FDA shut them down for 11 months.
Common Pitfalls and How to Avoid Them
Here’s what goes wrong-and how to fix it:
- Environmental neglect: 57.8% of calibration failures happen when temperature or humidity shifts more than ±5°C from calibration conditions. Solution: Install sensors in critical areas. Link them to alerts. Don’t assume your AC is enough.
- Documentation overload: Small manufacturers spend 15.2 hours a week just managing calibration records. Solution: Use cloud-based software like GageList or Trescal. Automate certificate generation, reminders, and audit trails.
- Legacy system integration: 32.7% of negative reviews cite problems syncing calibration data with SAP or other ERP systems. Solution: Choose software with API access. Don’t rely on manual CSV uploads.
- Assuming manufacturer specs are gospel: The manufacturer says calibrate every 6 months? Test it. If your data shows stability at 12 months, change the interval. Document the change. That’s compliance.
One semiconductor plant in Johannesburg had 41.3% of calibration failures due to uncontrolled humidity. They spent $100,000 on an ISO Class 5 environmental chamber. Failures dropped to 2%. ROI in 8 months.

What’s Changing in 2025 and Beyond
Regulations aren’t standing still. In March 2024, ISO published Amendment 1 to ISO 13485:2016-requiring calibration of AI and machine learning systems used in measurement. That’s new. If your quality control uses an algorithm to predict defect rates based on sensor data, you need to validate that algorithm’s drift over time. It’s not enough to calibrate the sensors. You have to monitor the AI.
The FDA’s 2024 Calibration Modernization Initiative mandates electronic records for all Class II and III device manufacturers by December 31, 2026. Paper logs are officially obsolete. If you’re still using binders, you’re already behind.
NIST is working on quantum-based standards that could make electrical measurements 100x more accurate by 2030. That means future calibration intervals could stretch from months to years-for the right tools.
But here’s the catch: 83.6% of calibration labs report technician shortages. In 2023, 47 accredited labs shut down because they couldn’t hire qualified staff. If you’re outsourcing, vet them hard. Ask for their ISO 17025 certification. Check their traceability chain. Don’t assume they know what they’re doing.
Who Needs This Most-and What It Costs
Medical device manufacturers face the strictest rules. 98.2% of ISO 13485-certified companies maintain full calibration programs. General manufacturers? Only 76.4%. But that gap is closing. With FDA inspections rising 17.4% annually, even food and automotive suppliers are tightening up.
Costs vary. Large companies spend 8-12% of their quality budget on calibration. Small ones (<50 employees) pay 22.3% more per device due to no volume discounts. But the real cost isn’t the calibration-it’s the failure.
A single recall in the medical device space can cost $5 million to $50 million. Calibration? $50,000 a year. That’s not an expense. It’s insurance.
Where to Start
If you’re starting from scratch, here’s your 6-month plan:
- Month 1-2: Inventory every measuring device. Give each one a unique ID. Note its function, tolerance, and usage frequency.
- Month 3: Classify by risk. High-risk = monthly or pre-use. Low-risk = yearly. Use the Method 5 approach: manufacturer recommendation + historical data + risk assessment.
- Month 4: Choose a calibration management system. Cloud-based. Automated. Integrates with your ERP.
- Month 5: Train your team. ASQ’s Certified Calibration Technician (CCT) course is a good baseline. NCSL International’s MET-101 covers the fundamentals.
- Month 6: Run a pilot. Pick one line. Validate the process. Document everything. Then scale.
Don’t wait for an audit to find your gaps. Start now. The cost of doing nothing isn’t just financial. It’s reputational. And sometimes, it’s fatal.
What’s the difference between calibration and validation?
Calibration checks if a measuring instrument reads accurately against a known standard. Validation confirms that a whole process or system works correctly under real-world conditions for its intended use. Calibration is about accuracy. Validation is about performance.
How often should I calibrate my equipment?
There’s no universal answer. ISO 13485:2016 requires calibration at specified intervals or before use. Intervals depend on risk, usage, environment, and historical data. A torque wrench in a cleanroom might need monthly checks. A basic thermometer in a warehouse might be fine annually. Use data-not guesswork-to set your schedule.
Can I use the manufacturer’s calibration certificate?
Only if it includes full traceability to SI units and documented measurement uncertainty. Many manufacturer certificates lack this. If you can’t trace the standard back to NIST or BIPM, it’s not compliant. Always verify the certificate’s details-not just the stamp.
What happens if I don’t calibrate my equipment?
You risk non-conforming products, customer complaints, regulatory fines, and recalls. In medical manufacturing, this can lead to patient harm. The FDA cited inadequate calibration in 37.2% of warning letters from 2020-2023. Audits will flag you. Insurance may deny claims. Reputational damage can be permanent.
Is calibration software worth the investment?
Yes-if you have more than 20 devices or multiple locations. Software like GageList or Trescal reduces audit prep time by 63%, cuts manual errors, and ensures compliance. Small manufacturers report saving 15+ hours per week on documentation. The ROI is clear: less time chasing paperwork, more time preventing failures.
Do I need to validate software used in calibration?
If the software is used to control, record, or analyze measurement data for quality purposes, yes. Under FDA 21 CFR Part 11 and ISO 13485:2016, software must be validated-even if it’s off-the-shelf. You need proof the algorithm doesn’t alter results. Don’t assume the vendor’s validation is enough-verify it yourself.



Alvin Montanez
December 13, 2025 AT 20:22Let me tell you something straight - if your company thinks calibration is just a yearly checkbox, you’re one FDA inspection away from a shutdown. I’ve seen it happen. A med device plant in Ohio lost their certification because they used a torque wrench that hadn’t been checked since 2021. The operator said, ‘It’s always been fine.’ Fine? It was off by 18%. That’s not ‘fine,’ that’s a liability waiting to happen. And don’t even get me started on vendors who send you certificates without traceability. That’s not compliance - that’s theater. ISO 13485 isn’t a suggestion. It’s a legal requirement. If you’re not documenting uncertainty values, you’re not just cutting corners - you’re putting lives at risk. Every time you skip a calibration because ‘it’s been working,’ you’re gambling with someone’s health. And guess what? The patient doesn’t care if your budget is tight. They just want to live. Stop pretending this is about paperwork. It’s about ethics. And if you’re not living up to it, you don’t belong in manufacturing. Period.
Lara Tobin
December 14, 2025 AT 08:48This hit me right in the feels 😔 I work in a small lab and we’ve been struggling to keep up with documentation. I’m not a compliance expert - I just want to make sure our devices work safely. Thank you for laying this out so clearly. I’m going to print this out and share it with our team tomorrow. We’ve been using that ‘it’s always been fine’ excuse too much. Time to change. 💪
Keasha Trawick
December 15, 2025 AT 17:13Ohhh honey, let me tell you about the calibration circus I inherited last year. We had a pH meter that was ‘calibrated’ by a guy who stamped ‘OK’ on a Post-it note. 18 months of drift. 47 failed batches. $220K down the drain. And the kicker? The vendor’s certificate had NIST stamped on it - but the traceability chain stopped at ‘some guy in a basement in Nebraska.’ 🤦♀️ We switched to GageList, automated the reminders, linked environmental sensors to Slack alerts, and now our calibration logs look like a NASA mission log. The audit team actually *complimented* us. That’s right - COMPLIMENTED. The real magic? Data. Not vibes. Not vendor promises. DATA. If your algorithm’s predicting defects, you better validate the damn algorithm, not just the sensor. AI doesn’t care about your ‘trust’ - it only cares about drift. And trust me, it drifts. Hard.
Scott Butler
December 16, 2025 AT 22:23Why are we letting foreign standards dictate how American manufacturers operate? NIST? ISO? Please. We built this country on ingenuity, not paperwork. If your equipment works, why does it need a certificate from some EU bureaucrat? I’ve seen American plants shut down because they didn’t have a humidity log from 2022. Meanwhile, factories in China and India are pumping out better products with no documentation. We’re suffocating ourselves with red tape. The FDA doesn’t need more rules - they need to stop harassing honest workers. Just fix the damn machine and move on. This is why manufacturing is leaving the U.S.
Emma Sbarge
December 17, 2025 AT 17:02Scott, your comment is dangerous and irresponsible. This isn’t about ‘red tape’ - it’s about preventing a child from getting a faulty pacemaker because a sensor drifted. You think China’s manufacturing is better? They had 120 medical device recalls last year. We’re not here to compete on cost - we’re here to save lives. If you can’t see that, you shouldn’t be in this industry. I’ve audited 47 facilities. The ones that cut corners? They all say the same thing: ‘It’s always worked.’ Then someone dies. And suddenly, ‘ingenuity’ looks a lot like negligence. Stop romanticizing shortcuts. This isn’t a debate. It’s a moral imperative.
Donna Hammond
December 18, 2025 AT 12:36For everyone still using paper logs - please, just stop. I’ve been in this field for 22 years, and I’ve seen the transition from binders to cloud systems. The difference? One saved a company from a $3M recall. The other got them a 11-month shutdown. Cloud-based tools like Trescal and GageList aren’t luxuries - they’re lifelines. They auto-generate certificates, send reminders, flag environmental breaches, and create audit trails that even the FDA can’t argue with. And yes, they cost money - but they pay for themselves in reduced downtime, fewer recalls, and less stress. I’ve helped three small manufacturers switch last year. One went from 15 hours a week on paperwork to 2. That’s 650 hours a year you can spend fixing real problems, not filing forms. Don’t wait for a warning letter. Start today. Your team - and your patients - will thank you.
Richard Ayres
December 19, 2025 AT 16:52There’s a lot of strong opinions here, and I appreciate the passion. But let’s not forget the human element. The technician who forgets to log a calibration because they’re short-staffed? The lab manager who doesn’t know how to interpret uncertainty values? We’re not just talking about compliance - we’re talking about support systems. Maybe the answer isn’t just better software, but better training, mentorship, and culture. I’ve seen teams turn things around not by buying new tools, but by sitting down together, asking ‘What’s making this hard?’ and fixing the process - not just the paperwork. The FDA doesn’t want to shut you down. They want you to protect people. Let’s build systems that help people do that - not just punish them when they slip.
kevin moranga
December 21, 2025 AT 06:19Hey everyone - I just want to say this: You’re all doing amazing work, even if it feels overwhelming right now. I used to think calibration was a nightmare too - until I started celebrating the small wins. One team calibrated their last 12 tools without a single failure. That’s huge. One lab cut their audit prep time from 3 weeks to 3 days. That’s a win. And that biomedical engineer in Durban who saved $18K? She didn’t wait for permission - she collected data, made a case, and changed the system. That’s leadership. You don’t need to be perfect. You just need to be consistent. Start with one tool. One sensor. One record. Build from there. And if you’re feeling stuck? Reach out. We’re all in this together. You’ve got this. 💪✨