Anticoagulant Procedure Risk Calculator
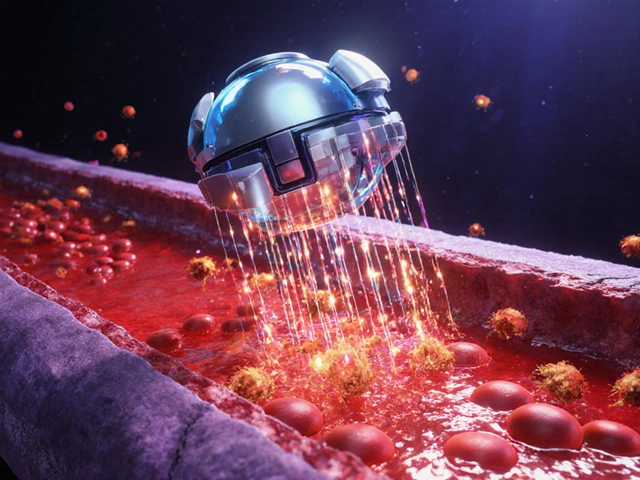
Why Your Blood Thinners Matter More Than You Think Before a Cosmetic Procedure
If you're taking a blood thinner-whether it's aspirin, warfarin, or a DOAC like rivaroxaban-and you're thinking about getting a cosmetic procedure, you’re not alone. About 25 to 40% of people seeing dermatologists or plastic surgeons for things like eyelid lifts, facial fillers, or skin resurfacing are already on some kind of anticoagulant. These medications help prevent strokes, heart attacks, and dangerous clots. But they also make you more likely to bruise, bleed, or form hematomas after a procedure. The big question isn’t whether to stop them-it’s when and how to manage them safely.
For years, the default advice was simple: stop your blood thinner before surgery. That changed after a landmark 1996 study by Dr. Otley showed that stopping warfarin or aspirin didn’t reduce bleeding complications in skin surgeries. In fact, stopping them often led to more serious problems-like strokes or pulmonary embolisms. A 2014 survey of 168 Mohs surgeons found 46 thromboembolic events after stopping anticoagulants, including 3 deaths. That’s not just a risk-it’s a preventable tragedy.
Not All Blood Thinners Are the Same
Trying to manage anticoagulants without knowing the difference between them is like trying to fix a car with the wrong wrench. There are three main types, and each behaves differently in your body.
- Antiplatelets (like aspirin and clopidogrel): These stop platelets from clumping. They’re the gentlest. Multiple studies, including one published in Skin Therapy Letter, show no significant increase in bleeding after minor cosmetic procedures-even when patients keep taking them.
- Warfarin: This older drug requires regular INR blood tests. If your INR is under 3.5, you’re generally safe to proceed with most procedures. But warfarin users have nearly 4 times higher odds of bleeding complications during facial surgeries, according to JAMA Facial Plastic Surgery. They’re also more likely to get infections afterward.
- Direct Oral Anticoagulants (DOACs) (rivaroxaban, apixaban, dabigatran): These are newer, faster-acting, and don’t need routine blood tests. Their half-lives are short-9 to 17 hours. For low-risk procedures, you can often just skip your morning dose on the day of surgery. For higher-risk ones, holding for 24 to 48 hours may be enough.
Here’s the kicker: stopping DOACs doesn’t reduce bleeding risk-it might even increase it. One study found 11 bleeding complications in patients who kept taking DOACs versus 3 in those who stopped. But the difference wasn’t statistically significant. Meanwhile, the risk of a clot forming after stopping? Around 0.15%. That’s low, but not zero. And for someone with atrial fibrillation or a mechanical heart valve, that 0.15% could be life-changing.
Procedure Type Determines Your Risk
Not every cosmetic procedure carries the same bleeding risk. Your doctor needs to know exactly what you’re getting done.
- Low-risk procedures: Shave biopsies, small excisions under 2 cm, Botox, dermal fillers, chemical peels, and laser treatments. For these, you should almost always keep taking your blood thinner. The bleeding risk is minimal, and stopping increases your chance of a clot far more than it reduces bruising.
- Moderate-risk procedures: Facial fat grafting, medium-depth chemical peels, some non-surgical body contouring. For DOACs, holding the morning dose is usually enough. For warfarin, ensure your INR is under 3.5. Antiplatelets? No need to stop.
- High-risk procedures: Facelifts, rhinoplasty, eyelid surgery (blepharoplasty), and Mohs surgery on the nose or lips. These areas are packed with blood vessels. Bleeding here can ruin results-causing asymmetry, scarring, or even blocking your airway. For these, your surgeon may ask you to pause DOACs for 24-48 hours. Warfarin might need to be stopped longer, with bridging only considered in rare cases.
One 2015-2022 study of 1,572 body contouring patients found only 1.27% had drug-related bleeding issues. Even then, the highest rate was with rivaroxaban (1.3%), and the lowest was with apixaban (0.48%). That tells you something: not all DOACs are created equal.
Why Bridging with Heparin Usually Makes Things Worse
You might hear about “bridging therapy”-switching from your oral anticoagulant to daily heparin injections before surgery. It sounds smart: keep you protected from clots while reducing bleeding risk. But here’s the truth: it doesn’t work well for cosmetic procedures.
Studies show bridging increases bleeding without lowering clot risk. The British Society of Dermatologists’ 2023 guidelines explicitly say: “Bridging is generally not recommended for minor and most moderate-risk procedures.” Why? Because you’re adding another anticoagulant on top of what you already have. That means more bruising, longer recovery, and higher chances of needing a second surgery to drain a hematoma.
There are exceptions-like patients with mechanical heart valves or recent clots. But for most people getting a facelift or lip filler? Bridging is unnecessary, risky, and outdated.
What Happens If You Bleed Too Much?
Bleeding after a cosmetic procedure isn’t just about a few extra bruises. It can lead to:
- Large hematomas that need to be drained
- Delayed healing and scarring
- Loss of skin grafts or flaps
- Permanent asymmetry (especially in eyelids or lips)
- Emergency room visits
- Return to the operating room
And if you’re on warfarin? You’re more likely to get an infection too. One study found warfarin users had over 7 times higher risk of post-op infection compared to those not on blood thinners. That’s not just a cosmetic issue-it’s a medical emergency.
That’s why prevention matters more than cleanup. The goal isn’t to avoid all bruising-it’s to avoid serious bleeding that changes your outcome forever.

What You Should Do Before Your Appointment
You’re not powerless here. Here’s your action plan:
- Don’t stop anything on your own. Never stop aspirin, warfarin, or DOACs without talking to your prescribing doctor and your cosmetic provider together.
- Bring your full medication list. Include doses and how long you’ve been taking each drug. Don’t forget supplements-fish oil, ginkgo, garlic, and vitamin E can also thin your blood.
- Ask for your INR if you’re on warfarin. Make sure it’s under 3.5 before scheduling. If it’s higher, your procedure may need to be delayed.
- Ask which category your procedure falls into. Low, moderate, or high risk? That tells you whether you need to pause your meds.
- Confirm the plan in writing. Get a clear, signed note from both your cardiologist and surgeon about what to do before, during, and after.
Many patients think, “I’ll just stop my pill for a few days.” But if you’re on DOACs, skipping one dose might be enough. If you’re on warfarin, you might need a blood test. If you’re on aspirin? You probably don’t need to do anything.
The Bottom Line: Stay on Your Meds Unless Told Otherwise
The old rule-stop everything before surgery-is dead. The new rule? Stay on your blood thinner unless your team says otherwise.
For most people getting minor cosmetic work, continuing your medication is safer than stopping it. Even for major procedures, stopping isn’t always the answer. The data is clear: the risk of a clot from stopping outweighs the risk of bruising from staying on.
Today’s best practice isn’t about blanket rules. It’s about matching your medication to your procedure, your health, and your risk level. It’s about teamwork between your cardiologist, dermatologist, and plastic surgeon. And it’s about understanding that a little extra bruising is far better than a stroke.
If you’re on anticoagulants and thinking about a cosmetic procedure, don’t assume you can’t have it. You can. You just need the right plan-and the right team.
Can I keep taking aspirin before a facelift?
Yes. Multiple studies show aspirin does not significantly increase bleeding risk in cosmetic procedures, even major ones like facelifts. Most surgeons now recommend continuing aspirin unless you’re having a procedure with extreme bleeding risk and your doctor advises otherwise. The risk of stopping aspirin-like triggering a heart attack or stroke-is far greater than the risk of extra bruising.
Should I stop my DOAC before a filler injection?
No. For filler injections, which are low-risk procedures, you should continue your DOAC. Skipping a dose is unnecessary and increases your clot risk. Studies show bleeding rates with DOAC continuation are around 1.74%, and stopping doesn’t lower that. The British Society of Dermatologists recommends continuing DOACs for all minor skin procedures.
What if my INR is 4.0? Can I still get a procedure?
If your INR is above 3.5, most surgeons will delay non-emergency procedures. An INR of 4.0 means your blood takes much longer to clot, raising your bleeding risk significantly. Your doctor may adjust your warfarin dose or temporarily reduce it to bring your INR down. Never try to fix this yourself. Work with your prescribing provider to get your INR into the safe range before scheduling.
Do I need to stop herbal supplements before surgery?
Yes. Many herbal supplements-like fish oil, ginkgo biloba, garlic, ginger, and green tea extract-can thin your blood. Even if you’re not on prescription anticoagulants, these can increase bruising and bleeding. Stop them at least 7-10 days before your procedure. Always tell your provider what supplements you take, even if you think they’re “natural” and harmless.
How long does bruising last after a procedure if I’m on blood thinners?
Bruising may last longer-up to 2-3 weeks instead of 1-2-especially with warfarin or DOACs. But it’s usually not worse in severity. The key is managing expectations. If you’re on anticoagulants, plan for a slightly longer recovery. Use cold compresses, keep your head elevated, and avoid alcohol or NSAIDs (like ibuprofen) that can make bruising worse.
What Comes Next?
If you’re on anticoagulants and considering a cosmetic procedure, the most important step is a conversation-not a decision made in isolation. Talk to your cardiologist, your dermatologist, and your surgeon together. Bring your lab results. Ask for the latest guidelines. Don’t accept a one-size-fits-all answer.
With the right approach, you don’t have to choose between safety and beauty. You can have both-without risking your life for a better look.




Rachel Wusowicz
November 14, 2025 AT 19:55ZAK SCHADER
November 16, 2025 AT 11:05Danish dan iwan Adventure
November 16, 2025 AT 17:01Ankit Right-hand for this but 2 qty HK 21
November 17, 2025 AT 05:26Oyejobi Olufemi
November 17, 2025 AT 15:01Latrisha M.
November 18, 2025 AT 10:03Jamie Watts
November 19, 2025 AT 01:26Daniel Stewart
November 20, 2025 AT 17:45