When your liver gets scarred, it doesn’t heal the way your skin does. Instead of repairing itself, it builds hard, fibrous tissue that slowly takes over. This is cirrhosis-the final, irreversible stage of chronic liver damage. It doesn’t come with a loud warning. Many people don’t feel sick until their liver is barely working. By then, the damage is deep, and the choices narrow: manage symptoms, avoid complications, or face the reality of needing a transplant.
What Happens Inside the Liver When Cirrhosis Develops
Your liver is a powerhouse. It cleans your blood, makes proteins, stores energy, and breaks down toxins. But when it’s under constant attack-whether from alcohol, hepatitis, or fat buildup-it tries to repair itself. Each time it heals, it leaves behind a bit of scar tissue. Over years, those scars pile up. Healthy liver cells get squeezed out. Blood flow slows. The organ’s structure turns into a maze of hard knots and fibrous bands. This isn’t just about feeling tired. The scar tissue blocks the tiny blood vessels inside the liver, raising pressure in the portal vein. That’s called portal hypertension. It leads to fluid leaking into the belly (ascites), enlarged veins in the esophagus that can burst (varices), and an enlarged spleen that traps platelets. Your liver can’t make enough albumin anymore, so your body starts holding onto water. Clotting factors drop, making you bruise easily. Toxins like ammonia build up in your blood and fog your brain-this is hepatic encephalopathy. The liver can handle a lot of damage before it fails. That’s why cirrhosis often flies under the radar. You might have normal blood tests for years. But once the scarring crosses a threshold, things unravel fast. The difference between compensated and decompensated cirrhosis is the line between survival and crisis.Compensated vs. Decompensated Cirrhosis: The Critical Divide
Compensated cirrhosis means your liver is scarred, but it’s still doing enough to keep you alive without obvious symptoms. You might feel fine. Your labs might look okay. But the damage is there. Studies show people in this stage have an 80-90% chance of living five more years-if they stop drinking, control their weight, and get treated for hepatitis. Decompensated cirrhosis is when the liver can’t keep up anymore. That’s when symptoms hit hard: swelling in the legs and belly, vomiting blood from burst veins, confusion or memory loss from toxins, and jaundice (yellow skin and eyes). At this point, survival drops to 20-50% over five years. No medication can reverse this. No supplement will fix it. The only real option left is a transplant. Doctors use two main tools to measure how bad it is: the Child-Pugh score and the MELD score. Child-Pugh looks at bilirubin, albumin, INR, ascites, and brain function. Scores range from A (mild) to C (severe). MELD uses bilirubin, creatinine, and INR to predict death risk in the next three months. A MELD score above 15 means you’re in serious danger without a transplant. A score above 20? You’re on the urgent list.What Causes Cirrhosis-and Why It’s Getting Worse
For decades, alcohol was the #1 cause. Now, it’s not even close. Non-alcoholic fatty liver disease (NAFLD) has taken over. One in four adults in the U.S. has fat in their liver. About 24% of cirrhosis cases now come from this. It’s tied to obesity, diabetes, and high cholesterol. It’s silent. You might not know you have it until you’re diagnosed with cirrhosis during a routine checkup. Hepatitis B and C used to be the big killers. Hepatitis C is now curable with 8-12 weeks of pills. But many people were never tested. They lived with it for 20 years, slowly scarring their liver. Hepatitis B is harder to cure, but vaccines and antivirals can stop it from progressing. Other causes include autoimmune liver disease, blocked bile ducts, genetic disorders like hemochromatosis, and long-term use of certain medications. In many cases, it’s a mix-someone drinks a little, eats too much sugar, and has undiagnosed hepatitis. The damage adds up.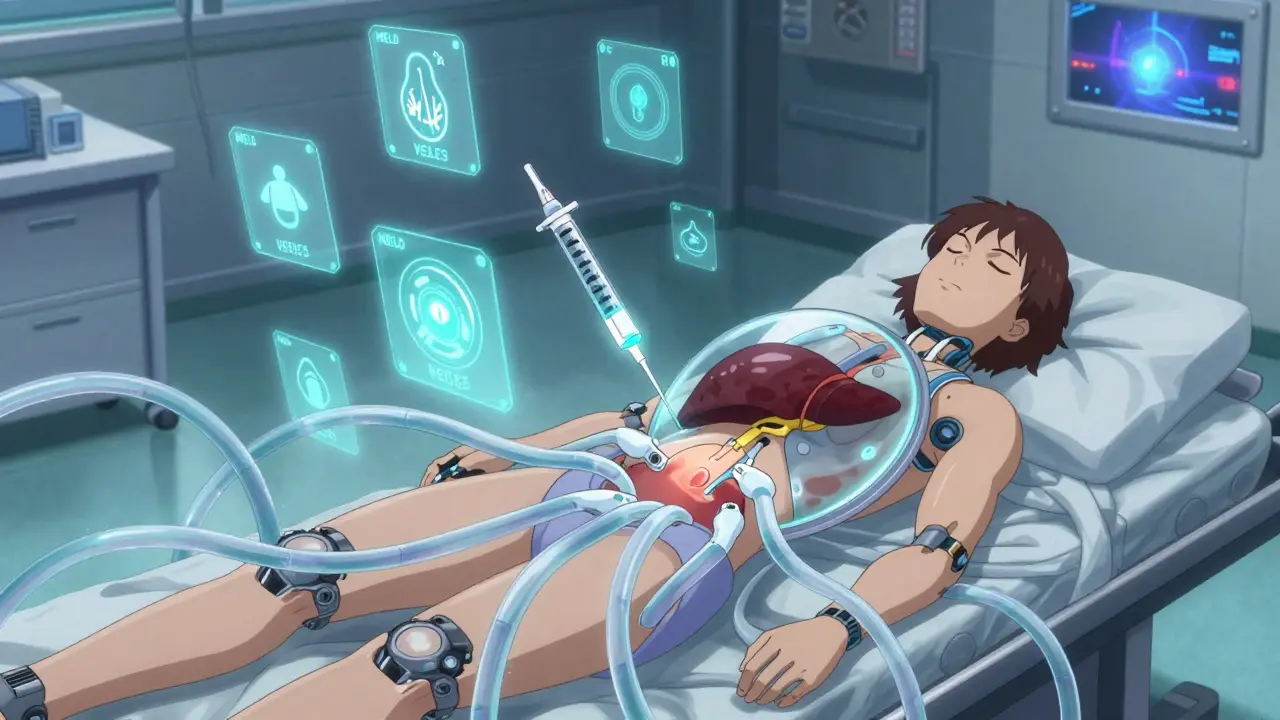
How Doctors Diagnose Cirrhosis Today
You won’t get diagnosed by feeling bad. You get diagnosed because your doctor saw something odd in your blood work. Elevated liver enzymes (ALT, AST) are the first red flag. Low platelets, high bilirubin, low albumin-they all point to trouble. Imaging helps. An ultrasound can show a lumpy, shrunken liver. A special type called elastography measures stiffness. A reading over 12.5 kPa strongly suggests cirrhosis. MRI elastography is even more accurate-90% correct in spotting advanced scarring. Liver biopsy used to be the gold standard. It’s still used sometimes, but now most diagnoses are made without surgery. Blood tests like FibroTest or ELF score can estimate scarring by measuring proteins linked to fibrosis. They’re not perfect, but they’re safer and good enough for most cases. The problem? Many people don’t get tested until it’s too late. A 2022 survey found 68% of cirrhosis patients waited six months or longer to get diagnosed after symptoms started. Fatigue? They thought it was stress. Belly swelling? They blamed weight gain. By the time they saw a specialist, the liver was failing.Managing Cirrhosis: What Actually Works
There’s no cure for cirrhosis. But you can stop it from getting worse. And you can prevent the worst complications. First, remove the cause. Stop drinking alcohol-completely. Lose weight if you’re overweight. Control diabetes. Take antivirals if you have hepatitis B or C. That’s it. That’s the foundation. Then, manage the fallout. Salt intake must be under 2,000 mg a day. Too much salt makes fluid build up. Diuretics help, but they’re not enough. If you have ascites, you might need a procedure to drain the fluid from your belly. Every liter removed needs 6-8 grams of albumin infused afterward, or your blood pressure can crash. Hepatic encephalopathy? That’s treated with lactulose or rifaximin. Lactulose pulls ammonia out of your gut. Rifaximin kills the bacteria that make it. Both help clear the brain fog. Avoid NSAIDs like ibuprofen. They hurt the kidneys, which are already under stress. Use acetaminophen (Tylenol) instead-but no more than 2,000 mg a day. And get vaccinated for hepatitis A and B, pneumonia, and the flu. Your immune system is weak. Most people need to see a liver specialist (hepatologist) regularly. But only 35% of rural U.S. counties have one. That’s a huge gap. If you can’t get to a specialist, your primary doctor needs to know how to monitor you: every 6 months for ultrasounds to check for liver cancer, every 3 months for blood tests.