When your doctor writes a prescription for a brand-name medication, you might assume it’s the best option for you. But more often than not, the pharmacy hands you a generic pill instead - and you’re not always told why. This isn’t random. It’s the result of a systematic push from health insurers demanding cheaper alternatives, and providers are caught in the middle.
Why Insurers Push for Generics
Insurers don’t push for generic drugs because they dislike brand names. They do it because generics cost 80 to 85% less. The FDA confirms this. For example, a 30-day supply of brand-name Lipitor might cost $300. The generic version? Around $15. That’s not a small difference - it’s billions saved across the U.S. healthcare system every year. By 2022, 90% of all prescriptions filled in the U.S. were for generics, according to FDA data. That’s up from 50% in the early 2000s. Insurers built systems to make this happen: tiered formularies, mandatory substitutions, and step therapy protocols. If you need a brand-name drug, you often have to try the generic first - and fail - before they’ll approve the original. Some plans won’t cover the brand at all unless you jump through hoops. It’s not just about saving money. It’s about control. Pharmacy Benefit Managers (PBMs) like CVS Caremark and OptumRx - who manage drug benefits for 85% of insured Americans - now work directly with insurers. That means they’re not just negotiating prices. They’re deciding which drugs you can even access.How Providers Are Forced to Adapt
Doctors aren’t just prescribing anymore. They’re becoming insurance clerks. A 2023 MGMA survey found physicians spend an average of 16.9 minutes on each prior authorization request. That’s not patient time. That’s paperwork time. One provider in Minnesota spent 22 days fighting an insurer to get approval for a brand-name blood thinner after a patient had dangerous reactions to the generic. Two emergency visits happened while waiting. Many clinics now hire dedicated staff just to handle prior authorizations. Medium-sized practices spend over $112,000 a year per full-time employee on this alone. And it’s not just time - it’s frustration. Nearly 80% of providers say these requirements cause patients to skip or abandon treatment. Some doctors have learned to game the system. They now include clinical justification in every prescription for brand-name drugs - even when they don’t think it’s needed. One cardiologist on Reddit said this increased his prescription processing time by 40%. Others use templates: pre-written letters for common exceptions, like documented allergies or previous treatment failures. It’s not ideal. But it’s the only way to keep up.The Tech Behind the Pressure
The real shift happened when insurers moved from paper forms to electronic prior authorization (ePA). In 2024, CMS made it mandatory for Medicare Advantage and Medicaid plans to use standardized ePA systems by 2027. That sounds good - until you realize how messy the system is. Each insurer has its own rules. One might require lab results showing a generic failed. Another might need a signed letter from the patient. And none of them define “medical necessity” the same way. A 2023 MGMA survey found 89% of physicians have to learn a new set of rules for every major insurer they work with. EHR systems are supposed to help. Some integrate with ePA platforms using HL7 FHIR standards. But not all do. And even when they do, approvals aren’t guaranteed. Approval rates for specialty drugs hover around 45%. For common conditions like hypertension, they’re closer to 85%. The difference? It’s not always clinical. It’s policy.
State Laws Are Starting to Push Back
Providers aren’t sitting still. States are stepping in. California’s AB 347, effective January 2024, forces insurers to approve step therapy exceptions within 72 hours if a doctor submits proper documentation. Approval rates jumped to 92% on first submission. That’s a game-changer. Arizona’s HB 2175, signed in May 2025, goes further. It bans insurers from using AI alone to deny care based on medical necessity. A human medical director must review each denial. Implementation starts June 2026. These laws aren’t outliers. In 2024 and 2025, 34 states introduced bills to limit prior authorization abuse. The federal Improving Seniors’ Timely Access to Care Act already requires Medicare Advantage plans to respond to urgent requests within 72 hours. But the patchwork remains. A provider in Florida might face one set of rules. In Texas, another. In Canada, mandatory substitution is more uniform - but even there, doctors report patients being switched to generics that cause side effects they didn’t have before.The Clinical Risks Nobody Talks About
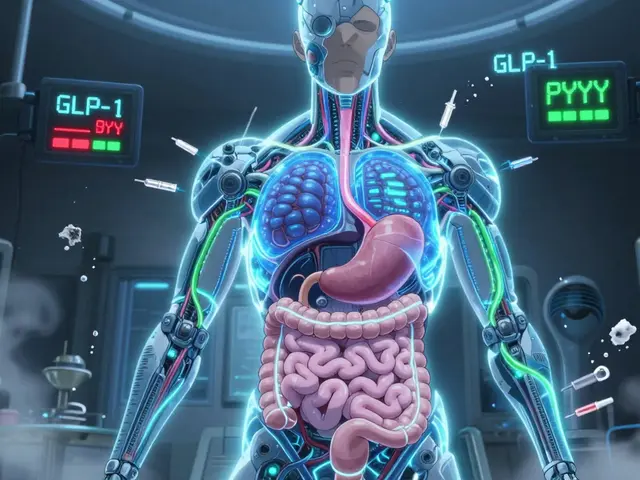
The FDA says generics must be bioequivalent within 80-125% of the brand-name drug’s absorption rate. That sounds precise - until you realize how wide that range is. For drugs like levothyroxine (used for thyroid conditions), small differences in absorption can cause serious problems. The AMA reports 28% of physicians have seen adverse outcomes after switching patients to a different generic version. Some patients develop new symptoms - fatigue, heart palpitations, weight gain - because the new pill just doesn’t work the same way. One psychiatrist in California told a forum: “I had a patient on the same brand-name antidepressant for seven years. Switched her to generic because the insurer forced it. She had a panic attack two days later. Took three weeks to stabilize her.” Insurers point to internal data showing 98.7% of substitutions proceed without issue. But that’s not the whole story. What about the 1.3%? That’s thousands of people. And for them, it’s not a statistic - it’s a health crisis.
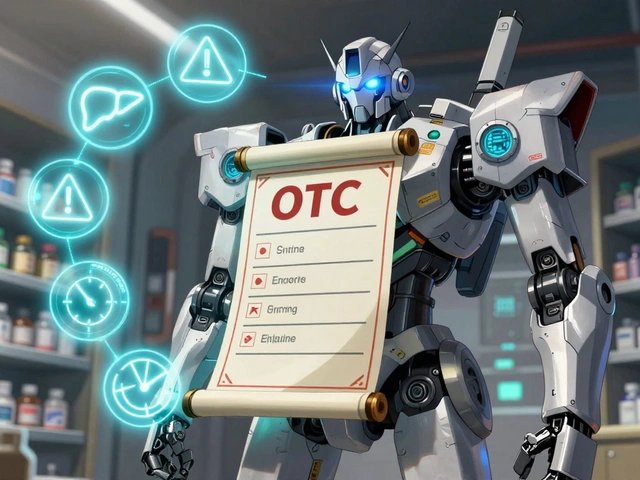
What Providers Are Doing Differently Now
Some doctors are changing how they practice. They’re “gold carding” - qualifying for exemptions from prior authorization by demonstrating high compliance and low denial rates. But only 5% of providers qualify. Others are building relationships with specific insurer case managers. A quick phone call can sometimes bypass a 10-day wait. A growing number are using AI tools to predict which prescriptions will be denied - not to replace judgment, but to prepare. They pre-load documentation before the patient even leaves the office. And more are refusing to prescribe brand-name drugs unless they’re absolutely necessary. “I used to write ‘do not substitute’ on every script,” one oncologist said. “Now I only do it when the patient’s life literally depends on it.”The Bigger Picture
The push for generics isn’t going away. UnitedHealthcare aims for 95% generic utilization by 2030. PBMs are investing billions in systems that make substitution automatic. But the backlash is growing. The AMA says prior authorization has caused patient deaths. Health economists warn that forcing switches undermines trust in doctors. And patients? They’re confused, frustrated, and sometimes sicker. The real question isn’t whether generics save money. They do. The question is: at what cost? If providers are forced to choose between following insurer rules and doing what’s best for their patients, someone’s going to lose. And too often, it’s the patient.What You Can Do as a Patient
If you’re handed a generic pill and feel something’s off - speak up. Ask your doctor: “Is this the same as what I was on?” “Can we check if the generic is approved for my condition?” Know your rights. In states like California, you can demand a fast exception. In others, you can appeal. Ask your provider to file it. Don’t assume a generic is always safe. If you’ve had a bad reaction before, document it. Bring lab results. Keep a journal of symptoms. And if your insurer denies coverage - don’t give up. One appeal can take weeks. But sometimes, it’s the only way to get the right treatment.Why do insurers force patients to use generic drugs?
Insurers mandate generic drugs because they cost 80-85% less than brand-name versions. This reduces overall healthcare spending. For example, a $300 brand-name drug can be replaced with a $15 generic. By 2022, 90% of prescriptions in the U.S. were for generics, largely due to insurer policies like tiered formularies and step therapy protocols that make brand-name drugs financially unattractive or inaccessible without approval.
What is prior authorization, and why is it a problem for providers?
Prior authorization is a process where doctors must get insurer approval before prescribing certain drugs - especially brand-name ones. It’s a problem because it adds hours of administrative work. Physicians spend an average of 16.9 minutes per request, and 78% report patients abandon treatment because of delays. Some cases take weeks to resolve, during which patients suffer worsening symptoms. The system also varies by insurer, forcing doctors to learn dozens of different rules.
Are generic drugs always safe and effective?
For most drugs, yes. The FDA requires generics to be bioequivalent within an 80-125% range of the brand-name drug’s absorption. But for drugs with a narrow therapeutic index - like levothyroxine, warfarin, or some seizure medications - even small differences can cause serious side effects. The AMA reports 28% of physicians have seen adverse outcomes after switching patients to a different generic version. Not all generics are identical in how they affect individuals.
Can patients fight insurer decisions to switch to generics?
Yes. Patients can appeal denials, especially if they’ve had documented adverse reactions to generics or if the brand-name drug is medically necessary. In states like California, providers can submit a standardized exception form, and insurers must respond within 72 hours for urgent cases. Successful appeals often include objective clinical data - lab results, prior treatment failures, or documented side effects - not just doctor opinions.
How are state laws changing how insurers handle generic substitution?
States are passing laws to limit insurer power. California’s AB 347 (2024) requires fast approval of step therapy exceptions. Arizona’s HB 2175 (2025) bans insurers from using AI alone to deny care. Thirty-four states introduced similar bills in 2024-2025. The federal Improving Seniors’ Timely Access to Care Act (2022) already mandates 72-hour responses for Medicare Advantage plans. These laws are forcing insurers to be faster, more transparent, and more human in their decisions.
What’s the future of generic substitution in healthcare?
Insurers plan to push for 95% generic use by 2030. But as more patients experience adverse effects and providers push back, regulators are stepping in. The FDA is reviewing complex generic drugs, with new guidance expected in late 2025. Electronic prior authorization will become mandatory nationwide by 2027, which may cut processing time by up to 60%. The trend will likely shift from blanket mandates to more nuanced rules - especially for drugs where small differences matter. The goal isn’t to eliminate generics, but to stop forcing them when they’re not safe.



Pankaj Singh
January 14, 2026 AT 01:36Insurers are just corporate vultures with spreadsheets. They don’t give a fuck about your thyroid or your depression-they care about Q3 margins. 85% cost savings? Cool. But when your patient has a panic attack because the generic version of sertraline has 2% less bioavailability, who gets sued? Not the PBM execs sipping lattes in Minneapolis.
Robin Williams
January 14, 2026 AT 02:08bro i just had my doc write 'do not substitute' on my script and the pharmacy still gave me the generic. i called the insurer and they said 'it was an error'... like i'm supposed to trust an error when my meds are literally keeping me alive? this system is broken. we need to burn it down and start over. #healthcareisnotabusiness
Scottie Baker
January 14, 2026 AT 18:02My doc just told me last week he’s not even writing prescriptions anymore-he’s writing appeals. He spends more time on phone calls with OptumRx than he does with patients. And guess what? He’s quitting private practice next year. This isn’t medicine anymore. It’s customer service with a stethoscope.
Anny Kaettano
January 16, 2026 AT 16:43Let’s not forget the clinical nuance here: bioequivalence ≠ clinical equivalence. For drugs with a narrow therapeutic index-levothyroxine, warfarin, phenytoin, carbamazepine-even minor PK/PD variations can trigger therapeutic failure or toxicity. The FDA’s 80-125% range is a statistical artifact, not a clinical guarantee. We’re treating patients like data points in a cost optimization algorithm, and that’s ethically indefensible.
Diana Campos Ortiz
January 18, 2026 AT 11:09i know this sounds dramatic but i had a friend switch to generic lamotrigine and she ended up in the er with a rash that turned into sjs. she’s fine now but it took 3 weeks and 4 hospital visits. the insurer said 'it was a coincidence'. no. it wasn’t. they never even asked if she’d had reactions before. just pushed the button.
Jesse Ibarra
January 19, 2026 AT 03:24Of course the 'patients' are 'confused'-they’ve been conditioned to think doctors are just glorified order-takers. Meanwhile, the real villains are the lazy, overpaid PBMs who think they can outsmart pharmacokinetics with a PowerPoint deck. If you're going to force a substitution, at least have the decency to pay for the damn lab work to prove it's safe. But no-let’s just let algorithms decide who lives and who doesn't. Classic American healthcare.
laura Drever
January 19, 2026 AT 06:20generic = cheaper. end of story. if you cant afford brand name then you aint getting it. stop whining. the system works. people are alive. thats all that matters.
Randall Little
January 20, 2026 AT 11:39So let me get this straight: a Canadian doctor can switch a patient to a generic and get away with it because the system’s standardized… but here, we’ve got 47 different insurer rulebooks, each written in a different dialect of bureaucratic nonsense? We’re not saving money-we’re wasting billions on administrative bloat. The real cost isn’t the pill. It’s the 16.9 minutes per prior auth. Multiply that by 1.2 billion prescriptions. That’s not efficiency. That’s insanity.
Acacia Hendrix
January 21, 2026 AT 09:01The empirical literature on generic substitution is overwhelmingly favorable for cost containment, yet the emotional anecdotes dominate the discourse. The 1.3% adverse event rate is statistically insignificant when weighed against the macroeconomic benefits of reduced drug expenditure. The real issue isn’t the generic-it’s the lack of longitudinal pharmacovigilance infrastructure to track individualized responses. Until we invest in that, we’re arguing semantics with anecdotal noise.
James Castner
January 22, 2026 AT 15:39It is imperative that we recognize the structural moral hazard embedded within the current pharmaceutical reimbursement paradigm. The conflation of fiscal responsibility with clinical autonomy has created a dystopian ecosystem wherein the physician-patient relationship is mediated by third-party administrators whose fiduciary duty lies not with health outcomes, but with shareholder value. The solution is not merely regulatory reform-it is a paradigmatic reorientation of healthcare delivery from a commodity-based model to a human-centered one. We must decouple therapeutic decision-making from financial incentives, and re-empower clinicians as stewards of patient welfare-not clerks for insurance algorithms. This is not merely policy-it is a moral imperative.
Adam Rivera
January 22, 2026 AT 15:45Hey, just wanted to say I’ve been on the same generic for 5 years now and it’s been fine. But I get it-some people have bad experiences. Maybe the answer isn’t banning generics, but making sure docs can easily flag high-risk patients. Like, a simple checkbox in the EHR: 'Has had reaction to generic X.' Simple. Fast. Saves lives. Why hasn’t this been done yet?